Centre for Ageing Better - Society | The State of Ageing 2023-24
May 2024 |
Centre for Ageing Better have published Society | The State of Ageing 2023-24, the chapter of their 'State of Ageing' report dealing with the social aspects of ageing in England today.
It is also possible to download a summary of the full report in pdf format.
Key findings in the current chapter include ...
- Civic and social participation
- Older people are more likely to vote than younger people, although this is also affected by social class with people from higher social grades (e.g. AB) more likely to vote at all ages.
- People aged 70 and over are just as likely to be concerned about climate change as young adults under 30, and people aged 50-69 are as likely to have made lifestyle changes because of these concerns as young adults under 30.
- Ageism
- Around half (46%) of people aged over 50 report experiencing ageism in the last year.
- Women are more likely than men to report ageism in relation to health or social care and media content.
- Unpaid Care
- Almost 3 million people aged 50 and over, in England, are unpaid carers
- People living in more deprived areas provide more hours of unpaid care and at younger ages than people living in less deprived areas.
- Local Communities
- Older people have a greater sense of belonging to their local area than younger people.
- Older people tend to have greater satisfaction with their area than younger people, but the people most likely to feel unsafe in parks and public spaces during the day are women aged 55 and over.
- Digital Inclusion
- The growing pace of digitalisation is leaving many older people behind.
- A quarter of people aged 65 and over do not have access to the internet at home.
- Having the essential digital skills may be becoming more of a barrier to older people than online access: only half of people aged over 75 have these skills and 43% of internet users aged 65 and over are limited in the activities they do online.
Centre for Ageing Better suggest that the UK government should establish a Commissioner for Older People and Ageing to deliver a strategy which gives a voice to the groups and issues currently marginalised, and ensure that policymaking across government considers the long-term needs of our ageing population.
|
Centre for Ageing Better - State of Ageing 2023-24
January 2024 |
Centre for Ageing Better have published their State of Ageing report 2023-24.
It is also possible to download a summary report in pdf format.
The Centre says that this year’s State of Ageing report paints the most detailed picture yet of the older population in England,using data from a variety of sources, including the 2021 Census.
Almost 40% of people in England are currently over 50,and almost 20% are over 65. There are almost three times as many people aged 85 and over as there were 40 years ago and the number of people aged 80 and over is set to more than double from 3 to 6 million in the next 40 years.
Contrary to the perception that all older people are well off and enjoy a comfortable retirement, almost one in five pensioners are living in relative poverty. Relative poverty among pensioners was at its lowest at 13% in 2012-13 but has been steadily increasing since then,reaching 18% in 2019-20 and remaining more or less at that level.
The report emphasises the links between health and poverty as well as regional and ethnic variations in health in older age.
It also looks at questions around employment in older age...
- The post pandemic recovery in employment rates for 50-64 year olds has been slow and the employment rate is still below its pre-pandemic peak.
- Those with higher incomes are much more likely to leave paid work early by choice; those on lower incomes are more often forced to leave due to health issues
- Many of those who fall out of the labour market in their 50s and 60s would like to return, but struggle to do so because of a variety of factors including caring responsibilities
- There’s a 15 percentage point gap between the employment rate of 35-49 year olds (86%) and 50-64 year olds (71%)
- There is also significant variation in employment rate by ethnic group. Among men aged 50-64, the ethnic groups with the lowest employment rates are Bangladeshi (65%) and Black Caribbean (68%), while the lowest rates for women are in Pakistani (29%) and Bangladeshi (20%) ethnic groups.
The report also looks at ageism and attitudes to ageing. It finds that people aged 50 and over are most likely to volunteer, vote and provide unpaid care, alongside the contributions they make to the economy through working and as consumers. Despite this, negative attitudes towards older people remain rife in the UK. One in three people has experienced ageism and the UK media has been found to be the most ageist of the 20 English-speaking countries analysed.
|
Institute for Fiscal Studies - The future of the state pension
December 2023 |
Institute for Fiscal Studies has published a report, The future of the state pension together with an Executive summary.
Today, individuals reaching state pension age (SPA) before 6 April 2016 are typically entitled to the flat-rate basic state pension (BSP, full amount currently £156.20 per week).
Those reaching the SPA on or after 6 April 2016 are typically entitled to the new state pension (nSP, full amount currently £203.85 per week).
While this report provides some background information on the historical evolution of the UK state pension, the analysis and recommendations focus on the nSP.
Key points include ...
- We are moving towards a flat-rate state pension which most people who spend most of their adult life in the UK will receive in full. The full new state pension is set at a level that means most new pensioners do not need to rely on the means-tested pension credit.
- There is widespread pessimism about the future of the state pension, and a mixture of confusion and pessimism about the level of the state pension.
- The triple lock increases the value of, and thus public spending on, the state pension relative to both prices and average earnings over time.
However Keeping the triple lock while raising the state pension age would hit poorer people more because the loss of a year of income is more important for those
with lower life expectancy, as they spend fewer years above the state pension age. On the other hand, those with a higher life expectancy benefit relatively more from the triple lock, as they are more likely to be receiving a generously indexed state pension in their 90s and beyond.
- The introduction of the new state pension in 2016 and (to a lesser extent) the triple lock since 2010 together have resulted in the full rate of the new state pension approaching 30% of median full-time earnings, higher than the basic pension was at any point since at least 1968.
- A more generous state pension would lead to a higher income for current and future pensioners and would be particularly valuable to low and middle income pensioners, but this would also have implications for public finances.
- There is a good case for simplifying the complicated eligibility rules and moving further towards a universal pension where essentially all people build entitlement to a state pension each year of life they live in the UK (up to a cap).
The report suggests a four point pension guarantee...
- A government target level for the new state pension, expressed as a share of median full-time earnings
- The state pension will continue to increase at least in line with inflation every year
- The state pension will not be means-tested
- The state pension age will only rise as longevity at older ages increases, and never by the full amount of that longevity increase.
|
Independent Age - Hidden renters - The unseen faces of the rising older rental wave
September 2023 |
Independent Age has published Hidden renters - The unseen faces of the rising older rental wave, a report which says that, while people of all ages rent privately, private renters on a low income in later life are a particularly vulnerable but largely hidden group.
The number of households in the private rented sector in the UK has increased significantly over the past decade, with those aged over 65 being one of the fastest-growing tenant groups. This trend is set to continue, with future generations of older people more likely to live in a rented home than they are today.
Renters of all ages in England can face a range of problems, including living in poor-quality properties, having a limited choice of rental properties, and concerns about being evicted and made homeless without any reason.
The research finds that almost two thirds of tenants over 65 have had to cut back on their general spending as a result of the cost-of-living crisis and rent increases. This is having a profound effect on their mental wellbeing, with more than half reporting feeling anxious about their finances.
Independent Age asks the UK government to commit to...
- Passing the Renters (Reform) Bill with longer eviction notices, better protection for people on benefits and measures to raise the standards of homes in the private rented sector
- Uprating Local Housing Allowance to ensure it covers at least the rent of the cheapest 30% of the local private rental market and to ensure that it is uprated annually to reflect changes in rents
- Providing local authorities with the power to moderate and cap in-tenancy rent increases
- Increasing government investment in social housing
- Giving more powers and funding to local authorities to improve enforcement of existing laws
|
HM Government - Next steps to put People at the Heart of Care
4 April 2023 |
HM Government has published a follow up to the December 2021 White Paper People at the Heart of Care called Next steps to put People at the Heart of Care - A plan for adult social care system reform 2023 to 2024 and 2024 to 2025.
The current plan includes key milestones for reform and sets out the changes so that older people can more easily draw on the care and support of unpaid carers, and those who work in social care.
Key activities include...
- Improving access to care and support, including helping local authorities to increase their adult social care capacity and make tangible improvements to services by investing £562 million in 2023 to 2024 and £845 million in 2024 to 2025 through the Market Sustainability and Improvement Fund.
- Recognising skills for careers in care, including improving recognition of the skills and experience of people working in care and supporting career development through a plan for the care workforce. This includes the introduction of a new care workforce pathway for adult social care, a new Care Certificate qualification, a skills passport to provide a verifiable record of training and qualifications and a range of new, funded training schemes.
- Digital transformation in adult social care. Supporting the testing and scaling of new technologies through 2023 to 2025 to improve care quality and safety; and increasing uptake of digital social care records by 2025, which enables care information to be shared securely and in real-time with authorised professionals in the NHS and social care.
- Personalising care through stronger data - introducing person-level data collection from April 2023.
- Improving transparency and accountability - introducing CQC assessment of local authorities’ adult social care delivery from April 2023
- Supporting people to remain independent at home - launching a new, independently chaired Older People’s Housing Taskforce that will make recommendations to ministers on how we can unlock investment in retirement housing to provide more choice of suitable housing for people in later life.
- Driving innovation and improvement - launching a 2-year targeted fund in 2023 to test and scale ways to innovate and transform local authority processes.
- Joining up services to support people and carers - supporting the recently established integrated care systems (ICSs), and the organisations within them, to better join up care through the expansion of our Better Care Fund (BCF) Support Programme and the launch of a new national leadership programme for local health and social care leaders.
The plan is seen as a crucial step towards a 10-year vision.
|
Institute for Fiscal Studies - How did increasing the state pension age from 65 to 66 affect household incomes?
20 June 2022 |
The Institute for Fiscal Studies has published How did increasing the state pension age from 65 to 66 affect household incomes?, an overall view of the effect of the change on older people's household incomes.
Key findings include...
- The biggest impact on incomes of the increase in the state pension age from 65 to 66 is simply that 65-year-olds lost, on average, state pension income worth around £142 per week in 2020-21.
- This reduction in state pension income was much larger than the overall increase in earnings arising from 65-year-olds delaying their retirement until they reached the new state pension age.
- Taking into account all forms of income, the increase in the state pension age pushed down the net income of 65-year-olds by an average of £108 per week.
- The reduced payments of state pensions, and the higher direct tax payments resulting from the increase in the state pension age, boosted the public finances by around £4.9 billion per year.
- The reductions in household incomes have had a particularly important effect on lower-income households: they have caused significant increases in income poverty rates among 65-year-olds.
- The reform caused absolute income poverty rates (after accounting for housing costs) among 65-year-olds to climb to 24%, some 14 percentage points higher than (more than double) the 10% that it is estimated it would have been had the state pension age remained at 65.
- For some groups, the increase in the state pension age from 65 to 66 caused absolute income poverty rates among 65-year-olds to rise by much more. This is because many in these groups were close to the poverty line prior to this increase in the state pension age.
- This latest increase in the state pension age led to a larger increase in income poverty than that seen following earlier increases in the female state pension age.
Most of the increase in absolute income poverty for 65-year-olds as a result of the reform has been among people not in paid work. The fraction of 65-year-olds who were in poverty and not in employment rose by 10 percentage points from a pre-reform baseline of 9%. However, there was also an increase in in-work poverty, with the share of 65-year-olds in work and in poverty rising by 3½ percentage points from a pre-reform baseline of only 1% of the 65-year-old population being in in-work poverty.
|
HM Government - Adult Social Care Reform White Paper - People at the Heart of Care
01 December 2021 |
Following its September 2021 Plan for adult social care reform in England, which set out future plans on how to pay for adult social care, the current white paper introduces a broader 10-year plan for adult social care across the life course.
The white paper emphasises person-centred care as a key theme running through the vision, providing genuine choice and control about personalised care and support to "enhance quality of life and promote independence in a way that matters to individuals".
The white paper identifies a number of key areas for future action and expenditure:
- At least £300 million to integrate housing into local health and care strategies, with a focus on increasing the range of new supported housing options available. This will provide choice of alternative housing and support options.
- At least £150 million of additional funding to drive greater adoption of technology and achieve widespread digitisation across social care. Digital tools and technology can support independent living and improve the quality of care.
- At least £500 million so the social care workforce have the right training and qualifcations, and feel recognised and valued for their skills and commitment. We want the workforce to also have their wellbeing prioritised.
- A new practical support service to make minor repairs and changes in peoples' homes to help people remain independent and safe in their home, alongside increasing the upper limit of the Disabilities Facilities Grant for home adaptations such as stairlifts, wetrooms and home technologies.
- Up to £25 million to work with the sector to kick start a change in the services provided to support unpaid carers.
- £30 million to help local areas innovate around the support and care they provide in new and different ways, providing more options that suit peoples' needs and individual circumstances.
- A new national website to explain the upcoming changes and at least £5 million to pilot new ways to help people understand and access the care and support available.
- More than £70 million to increase the support offer across adult social care to improve the delivery of care and support services, including assisting local authorities to better plan and develop the support and care options available.
These proposals are backed by the new Health & Care Levy announced in September.
|
HM Government - Policy paper - Adult social care charging reform: further details
18 November 2021 |
On 7 September 2021, the UK Government set out its Plan for adult social care reform in England. The plan included, from October 2023, a lifetime cap on personal care costs of £86,000. This cap excluded daily living costs. The current update clarifies a number of issues including that Daily living cost will be set as a national, notional amount of £200 per week, which will apply to anyone who receives care in a care home.
|
Carers UK - State of Caring 2021 - A snapshot of unpaid care in the UK
20 October 2021 |
Carers UK have published State of Caring 2021 - A snapshot of unpaid care in the UK an annual survey of carers to help understand the state of caring in the UK.
Carers UK carried out an online survey between August and September 2021. A total of 8,676 carers and former carers responded to the survey, of whom 8,119 people who currently provide care are included in the report.
Of these ...
- 79% identify as female, 19% identify as male and 0.5% describe their gender identity in another way.
- 28% consider themselves to have a disability.
- 3% are aged 0-34, 10% are aged 35-44, 23% are aged 45-54, 36% are aged 55- 64, 20% are aged 65-74, and 7% are aged 75 and over.
- 3% identified as lesbian, gay or bisexual.
- 4% described their ethnicity as Black or minority ethnic.
- 16% also have childcare responsibilities for a non-disabled child under 18
- 34% are in paid work. Of those, 46% work full-time and 39% part-time.
- 33% have been caring for 15 years or more, 15% for between 10-14 years, 23% for 5-9 years, 26% for 1-4 years, and just 3% have been caring for less than one year
- 48% care for 90 or more hours every week, while 14% care for 50-89 hours, 23% care for 20-49 hours, and 13% care for 1-19 hours a week.
- 76% care for one person, 18% care for two people, 4% for three people, and 2% care for four or more people.
The report also looks at the continued impact of the Covid-19 pandemic on carers' ability to juggle work and care -
- Working carers represent a significant proportion of the working population and at the height of the pandemic, Carers UK estimated that over a quarter (26%) of all workers were juggling work and care.
- There has been a significant move towards working from home either full- or part-time during the pandemic, with 47% of working carers now working from home either all or some of the time.
- The challenges of balancing work and care often have a negative effect on carers' careers, with previous research finding that 40% of working carers had passed on opportunities at work and 25% had moved roles to help them manage.
- Services being closed or reduced during the COVID-19 pandemic meant that some carers felt they had no choice but to reduce their hours or give up work.
|
Welsh Government - Age friendly Wales: our strategy for an ageing society
7 October 2021 |
The Welsh Government have published Age friendly Wales: our strategy for an ageing society, which sets out the actions they will take to "reap the benefits of the growing number of older people in Wales as we rebuild our communities".
The main aims of the strategy are: 1.Enhancing well-being; 2. Improving local services and environments; 3. Building and retaining people's own capability; and 4. Tackling age related poverty.
Helping to develop the overall strategy will be a number of contributory plans and strategies: Race Equality Action Plan; LGBTQ+ Action Plan; National Framework for Bereavement Care; Transport Strategy; Advancing Gender Equality in Wales Plan; A Healthier Wales; Strategy for Unpaid Carers; Together for Mental Health; Dementia Action Plan; Healthy Weight - Healthy Wales Strategy; Action on Disability - the Right to Independent Living; Cymraeg 2050; Connected Communities - A Strategy for tackling loneliness and isolation.
To monitor progress the Welsh Government have established a Ministerial Advisory Forum and will work with the forum to draft a delivery plan which will set out actions, milestones and timescales by which progress can be measured. The intention is to publish annual progress reports. The Welsh Government have commissioned and produced the UK Age Index for Wales, which has shaped the strategy and will be used to measure its success.
|
HM Government - Build Back Better
7th September 2021 |
On 7th September 2021, HM Government published Build Back Better, its plans for the immediate post-pandemic funding of health care and its longer term proposals for the funding of social care in England.
The announcement for social care is structurally similar to proposals in the 2011 Dilnot Commission report, although the numbers are different.
Key proposals include ...
- A lifetime cap of £86,000, per individual, on care cost charges (excluding residential accommodation costs)
- Fully paid for care for individuals with assets of less than £20,000
- Means tested support for individuals with between £20,000 and £100,000 in assets
To pay for this, from April 2022, Employer and Employee National Insurance contributions will each increase by 1.25% of income. From April 2023 this part of National Insurance contributions will be identified as a separate, notionally hypothecated, charge - the Health and Social Care Levy, which will, unlike National Insurance, continue to be paid after state pension age.
In addition, shareholders will pay an extra 1.25% tax on their profits.
The measures are expected to raise £12bn per year which will initially (2-3 years) go towards funding the National Health Service to help clear backlogs caused by the Covid pandemic. A proportion of this tax revenue will go to the devolved administrations in Scotland, Wales and Northern Ireland to spend in line with local policies.
Before the end of 2021, HM Government will publish a White Paper, setting out its proposals for the reform of social care and its better integration with health care in England
|
UK Parliament, House of Commons / House of Lords, Joint Committee on Human Rights - Care homes: Visiting restrictions during the covid-19 pandemic 5th May 2021 |
The House of Commons / House of Lords, Joint Committee on Human Rights have published their fifteenth report of session 2019-21 on Care homes: Visiting restrictions during the covid-19 pandemic.
Since the start of the covid-19 pandemic, official guidance on care home visiting has prioritised the duty to protect residents' right to life, even where this has severely impacted the right to respect for private and family life.
Over the last 14 months, family members, many of whom perform essential care giving roles,were either banned from visiting their loved ones or faced very significant limitations on their ability to be with them.
The committee heard numerous reports of people suffering rapid declines in their physical and mental health as they were isolated from their families for over a year.
The report finds that while the Government has a duty to protect the lives of residents in care homes, it also has an obligation to uphold their right to family life and ensure this is facilitated in practice.
Although Government guidance (England only), has begun to reflect the importance of allowing care home residents to be with their families and makes clear that care home providers should not impose blanket bans on visiting, the Government’s guidance does not have statutory force.
The report reiterates the committee's call for legislation to require that individualised risk assessments are undertaken for each resident.
|
Archbishops of Canterbury and York - Commission on Reimagining Care
19th April 2021 |
The Archbishops of Canterbury and York have announced a new Commission on Reimagining Care aimed at developing a radical and inspiring vision, drawing on Christian theology and tradition, that reimagines care and support. The Commission will set out proposals to achieve this vision.
The Commission is chaired by Dr Anna Dixon, former chief executive of the Centre for Ageing Better.
It aims to articulate the enduring values and principles which should underpin care and caring. It will seek to shape how we respond to ageing and disability in our society, challenging existing attitudes and models of care, where appropriate, and highlighting the positive and where things are working well.
|
House of Commons Library - State Pension triple lock
4th February 2021 |
The House of Commons Library has published a briefing paper State Pension triple lock, summarising the background and possible future of the government commitment to uprate the basic and new State Pension by the highest of earnings, prices or 2.5%.
The State Pension for people who reached State Pension age (SPA) before 6 April 2016 has two tiers:
the basic State Pension (bSP) - based on a person’s National Insurance contribution record; and
the additional State Pension - which is partly earnings-related.
A new State Pension (nSP) was introduced for future pensioners from 6 April 2016.
For the bSP and nSP, there is a statutory requirement to uprate every year at least in line with earnings. Different uprating arrangements apply to the other parts of the State Pension - such as the additional State Pension and the additional amounts earned by deferring a claim to the State Pension.
The triple lock is a government commitment, over and above the statutory requirement, to uprate the basic and new State Pension by the highest of earnings, prices, as measured by the Consumer Prices Index (CPI) or 2.5%. Its introduction was announced by the Coalition Government in its first Budget after the 2010 election
There was cross-party support for the triple lock in manifestos for the 2019 general election.
Although the triple lock was introduced by the Coalition Government in June 2010, its roots are in earlier developments - in particular the link with earnings under Labour in the 1970s which was subsequently broken by the Conservative Government in the early 1980s.
The triple lock has been effective. The full basic State Pension for an individual in 2021/22 will be
- 10.8% higher than if it had been CPI-indexed
- 10.3% higher than if it had been earnings-linked
- 3.8% higher than if it had been ‘double-locked’ in line with the higher of earnings or CPI
- In recent years the triple lock and the nSP have helped to also boost the core value of the State Pension relative to earnings. Following the introduction of the triple lock, by 2020, the value of the bSP had risen from 17% to 19% of average full-time earnings.
According to this briefing, arguments for and against the policy since its introduction have centred around questions of cost and intergenerational fairness.
Analysis by the Pensions Policy Institute in 2018 showed that the triple lock would increase the incomes of future pensioners (as well as today’s) and make it easier for them to achieve adequate retirement incomes by reducing the amount they needed to save privately.
The briefing also reviews a number of options for moderating the addition state pension expenditure generated by the triple lock.
|
European Commission - GREEN PAPER ON AGEING: Fostering solidarity and responsibility between generations
27th January 2021 |
The European Commission have published a Green Paper on Ageing: Fostering solidarity and responsibility between generations. The purpose of this green paper is to launch a broad policy debate on ageing, taking into account the UN 2030 Agenda for Sustainable Development and UN Decade for Healthy Ageing.
Competences for dealing with the effects of ageing are largely in the hands of Member States and the EU Commission feels it can help Member States and regions develop their own, tailor-made policy responses to ageing.
The green paper takes a life-cycle approach that reflects the universal impact of ageing and focuses on both the personal and wider societal implications of ageing.
The green paper focuses on healthy and active ageing, and lifelong learning, both of which work best when they start at an early age.
- Healthy and active ageing - promoting healthy lifestyles throughout our lives including consumption and nutrition patterns and the levels of physical and social activity.
- Lifelong learning - investing in people’s knowledge, skills and competences throughout their lives, including acquiring and updating skills which improve employability in working life, and continued learning in later life which may help to delay the onset of dementia and prevent cognitive decline related to old age.
The Green Paper looks at new opportunities and challenges in retirement including staying active through Volunteering, Intergenerational learning, and Walking and Cycling to maintain mobility. It considers the problems facing older people with disabilities and the need to maintain the autonomy, participation and rights of older people.
The Green Paper covers many of the diverse aspects of life in older age ranging from meeting the health and long-term care needs of an ageing population; mobility, connectivity and accessibility; and access to care and services; to the redistribution and fairness of pension systems.
Read CPA's response to the European Commission Green Paper on Ageing.
|
Office for National Statistics - Health state life expectancies, UK: 2017 to 2019
25th January 2021 |
The Office for National Statistics (ONS) have published Health state life expectancies, UK: 2017 to 2019.
The report looks at the number of years people are expected to spend in different health states among local authority areas in the UK.
Key points raised are ...
- This release is calculated based on figures prior to the coronavirus (COVID-19) pandemic and will not reflect the impact of the pandemic on health state life expectancies.
- In 2017 to 2019 healthy life expectancy (HLE) at birth in the UK for males was 62.9 years, showing no significant change since 2014 to 2016; however, HLE for females showed a significant decrease from 63.7 years in 2014 to 2016 to 63.3 years in 2017 to 2019.
- The gap in years lived in good health between males and females has narrowed since 2009 to 2011, largely as a result of female HLE being lower in subsequent periods.
- In 2017 to 2019, disability free life expectancy (DFLE) in the UK was 62.3 years for males and 61.0 years for females; there was a significant decrease of more than a year in DFLE since 2014 to 2016 for females, but no significant change was observed for males.
- Unlike at birth, there was a statistically significant increase in HLE at age 65 years for males in the UK rising from 10.2 years in 2014 to 2016 to 10.4 years in 2017 to 2019; female HLE also increased from 10.8 years to 11.0 years between the same periods but this was not statistically significant.
- DFLE at age 65 years in the UK showed no significant changes in 2017 to 2019 for either sex, at 9.7 years for males and 9.6 years for females.
Life expectancy estimates are calculated using all causes of death, and are calculated based on figures before the coronavirus (COVID-19) pandemic.
|
House of Lords - Science and Technology Select Committee - Ageing: Science, Technology and Healthy Living
15th January 2021 |
The House of Lords - Science and Technology Select Committee has published Ageing: Science, Technology and Healthy Living which looks at: the Demography of ageing, including life expectancy and mortality; Biological ageing including why humans age; the influences of lifestyle and environment; and how technology can help. The report also looks at the impact of COVID-19.
Key findings include...
- Life expectancy and mortality: Healthy life expectancy and disability free life expectancy have failed to keep pace with increases in life expectancy, particularly for women. This means more years, on average, spent in poor health. Ageing exacerbates the inequalities of earlier life with older people in the most deprived group spending, on average, 20 years longer in poor health than those on the least deprived group.
Multimorbidity is common, and is linked to socioeconomic deprivation, but the health service is designed and organised to deal with single conditions. Polypharmacy, the prescription of multiple medications by different doctors, heightens the risk of adverse drug reactions and an increased use of 'Comprehensive Geriatric Assessments' is suggested.
- Biological ageing: Ageing is the result of an "accumulation of a wide variety of molecular and cellular damage over time." This damage leads to decreased physical and cognitive capacity, and increasing risk of illness and death.
The report summarises the "mutation accumulation" theory, the "antagonistic pleiotropy" theory, and the "disposable soma" theory of biological ageing.
The nine hallmarks of biological ageing are: Genomic instability, Telomere attrition, Epigenetic alterations, Loss of proteostasis, Deregulated nutrient-sensing, Mitochondrial dysfunction, Cellular senescence, Stem cell exhaustion, and Altered intercellular communication.
The UK has historically been a major player in drug research and development, and has the potential to be a key player in the development of treatments targeting the processes of ageing. However, companies in the UK struggle to commercialise such innovations and often have to move abroad to access finance. .
The exclusion of people with multimorbidity from clinical trials is a particular issue for drugs targeting the ageing process.
- Lifestyle and the environment: The most significant risk factors affecting health outcomes in middle and older age are smoking, poor nutrition, obesity, insufficient physical activity and excessive alcohol consumption. There is consensus from cohort study data that lifestyle factors are strongly linked to lifespan and mortality. Healthy lifestyle behaviours, and positive lifestyle changes made at any stage in life, can increase healthy life expectancy.
Health throughout the life-course can be affected by the 'environment'. People can be harmed directly, for example by pollution. There is growing evidence that air pollution harms health in old age, including cognitive health.
The built environment affects health throughout the life-course. Poor quality housing contributes to ill health, for example dampness and poor air quality are associated with respiratory illnesses, and cold is associated with hypothermia.
There is evidence that physical activity tailored to the abilities of different groups of older people have benefits for health, for example reducing the risk of type 2 diabetes and mitigating some effects of rheumatoid arthritis. However, it is difficult to determine the exact contribution that physical exercise makes to health, and by what mechanisms.
Cognitive ability and psychological stresses are key aspects of health throughout the life-course, but they also influence general health and might affect the underlying processes of ageing.
- How technology can help: Technologies and related services have a role in helping people to live healthily and independently in old age. These include assistive technologies, which can compensate for declining ability and help individuals to cope better with their environment, and medical technologies, which can improve health and capability.
In order to improve uptake and usefulness of technologies and services that can contribute to healthier and independent living in old age, it is important to base the process of development and deployment around older people's needs, preferences and abilities. It is beneficial for older people to be involved in the design of these products and services.
- The impact of COVID-19: The COVID-19 pandemic has had disproportionate impacts upon older people, in terms of severity of disease and death rates. The population of England aged 65 and over is currently around 18%, but patients in that age group accounted for 60% of hospital admissions for COVID-19 (up to 30 September 2020). Patients aged 60 and over represented 92% of patients who died in hospitals having tested positive for COVID-19 (in England, up to 5 November 2020).
Recommendations include:
The Government clearly defines the roles and responsibilities for healthy ageing among national and local government and their agencies. The creation of the National Institute for Health Protection should be used as an opportunity to revitalise work to promote healthy ageing across the life-course, including by improving coordination across the sector and drawing on the best information for developing public health advice.
The Government implements a concerted and coordinated set of national policies to support healthy ageing, including: regulatory and fiscal measures, actively to encourage people to adopt lifestyles that support healthy ageing; increasing the reach of the NHS Health Check to those in disadvantaged groups who will benefit the most; and working with local authorities on the funding of local services, housing and infrastructure to encourage and facilitate healthier living across the life-course, including the necessary services to maintain health and independence in old age.
The Government ensures internet access for all homes so that older people can access services to help them live independently and in better health. The Government should promote and support lifelong digital skills training so that people enter old age with the ability to use beneficial technologies. Greater support should be provided to the large proportion of the current older generation which lacks these skills, so that they do not miss out on the benefits of available technologies.
|
The Centre for Ageing Better - The State of Ageing 2020
19th November 2020 |
The Centre for Ageing Better has published The State of Ageing 2020, a report which looks at the state of health, finances and communities when COVID-19 hit and the impact of the pandemic. It focuses on four key areas - work, housing, health and communities. .
Key points raised in the report include ...
- COVID-19 has laid bare the urgency of improving the state of ageing
- Even before the pandemic, progress on improving life expectancy was stalling – and disability-free life expectancy for women was going backwards
- Women in the wealthiest parts of the country are set to live 16 years longer in good health than those in the poorest
- More than two million people aged 55 or older are living in a home that endangers their health or wellbeing
- Only 9% of homes in England are visitable by people with accessibility needs
- COVID-19 risks bringing about a long-term unemployment crisis among the over 50s
- Lockdown has seen a surge in community activity – but in many cases the people who are struggling to get by are missing out
The report argues that we are on the path to a future of ageing badly but there are steps we can take to change this trajectory
|
World Health Organisation - Fact file: Misconceptions on ageing and health
July 2020 |
The World Health Organisation have produced a brief web-based fact file: Misconceptions on ageing and health.
Key themes examined include...
- There is no typical older person:
- Diversity in older age is not random:
- Only a small proportion of older people are care dependent: Research in the United Kingdom of Great Britain and Northern Ireland in 2011 estimated that, the contributions older people made through taxation, consumer spending and other economically valuable activities were worth nearly GBP 40 billion more than expenditure on them through pensions, welfare and health care combined
- Population ageing will increase health-care costs but not by as much as expected:
- 70 is not yet the new 60: There is little evidence that older people today are experiencing life in better health than was the case for their parents or their grandparents.
- Good health in older age is not just the absence of disease:
- Families are important but alone cannot provide the care many older people need:
- Expenditure on older populations is an investment, not a cost: These investments can yield significant dividends, both in the health and well-being of older people and for society as a whole through increased participation, consumption and social cohesion.
- It’s not all about genes: only approximately 25% of the diversity in longevity is explained by genetic factors
- Mandatory retirement ages do not help create jobs for youth:
|
European Commission - Report on the Impact of Demographic Change
17th June 2020 |
The European Commission have published their Report on the Impact of Demographic Change.
The report presents the drivers of demographic change and the impact they are having across Europe. It aims to 'help identify how the people, regions and communities most affected can best be supported to adapt to changing realities through crisis, recovery and beyond'.
The key drivers of demographic change in Europe are longer life expectancy, fewer births, an ageing population, smaller households, greater mobility, and a changing population size.
In the field of work, the report considers the growth of a larger and more inclusive labour market as well as improving productivity through skills and education. It also looks at the implications for health and long-term care.
The report also considers the geopolitics of demographics and Europe in the world. It looks at demographic change and the twin green and digital transitions, as well as climate change.
Relative population growth across the world means that Europe's share of the world population and global GDP is diminishing. The report concludes that 'the twin challenge of democracy and demography must be tackled head-on'.
|
Public Health England - Disparities in the risk and outcomes of COVID-19
2nd June 2020 |
Public Health England have published Disparities in the risk and outcomes of COVID-19 which outlines the key factors which lead to variations in the risks and outcomes from COVID-19.
COVID-19 often replicates existing health inequalities and, in some cases, increases them.
The largest disparity is age. Among people already diagnosed with COVID19, people who are 80 or older are seventy times more likely to die than those under 40.
Risk of dying among those diagnosed with COVID-19 is also higher in males than females; higher in those living in the more deprived areas than those living in the least deprived; and higher in those in Black, Asian and Minority Ethnic (BAME) groups than in White ethnic groups.
The analyses in the report take into account age, sex, deprivation, region and ethnicity, but do not take into account the existence of comorbidities, which are strongly associated with the risk of death from COVID-19 and are likely to explain some of the differences.
The analysis is of confirmed cases, mainly tested in hospital, and therefore represents people with severe disease, rather than all of those who get infected. It also does not take into account occupation which may explain some of the variations between social and ethnic groups.
Areas of disparity examined include ...
- Age and Sex: Working age males diagnosed with COVID-19 are twice as likely to die as females; A person aged 80 or over who tests positive is 70 times more likely to die than someone aged 40.
- Location: Areas with the highest rates of diagnosis and death are mainly urban; Death rates in London are three times higher than in the South West.
- Levels of deprivation: Mortality rates from COVID-19 in the most deprived areas are double those in the least deprived areas.
- Ethnicity: People of Bangladeshi ethnicity are twice as likely to die of COVID-19 than White British. Other minority ethnic groups have a 10-50% higher risk than White British.
- Occupation: A predominance of COVID-19 cases occurs among health workers and men who work as security guards, taxi drivers, chauffeurs, bus and coach drivers, and lower paid workers including sales and retail and social care workers.
- Country of birth and rough sleeping: Higher death rates are noted among people born overseas and those who have been rough sleepers.
- Care homes: All-cause deaths in care homes between 20 March and 7 May 2020 were more than double the expect rate with 20,457 excess deaths.
- Comorbidities: A high proportion COVID-19 related deaths also mention diabetes, hypertension kidney disease, COPD and dementia.
|
UK Government - Staying alert and safe (social distancing) - revised guidance
31st May 2020 |
The UK Government has published revised guidance which became operational in England from 1st June.
Some people, including those aged 70 and over, those with specific chronic pre-existing conditions and pregnant women, are considered clinically vulnerable. This group should continue to take particular care to minimise contact with others outside their household.
People who are defined, on medical grounds, as clinically extremely vulnerable to coronavirus - that is, people with specific serious health conditions - are advised to continue shielding to keep themselves safe by staying at home and avoiding gatherings or, if individuals wish to spend time outdoors, to take extra care to minimise contact with others by keeping two metres apart at all times.
|
UK Government - OUR PLAN TO REBUILD: The UK Government’s COVID-19 recovery strategy
11 May 2020 |
The UK Government has published OUR PLAN TO REBUILD: The UK Government’s COVID-19 recovery strategy. Because of the devolution of powers to Scotland, Wales and Northern Ireland, many of the shorter term proposals only apply to England.
The document outlines a phased approach towards returning to normal but emphasises that this is not a short-term crisis and it is likely that COVID-19 will circulate in the human population long-term, possibly causing periodic epidemics.
Throughout the next (second) phase, people will need to minimise the spread of the disease through continuing good hygiene practices: hand washing, social distancing and regular disinfecting of surfaces touched by others. These will be in place for some time.
The number of social contacts people make each day must continue to be limited, the exposure of vulnerable groups must continue to be reduced from normal levels, and symptomatic and diagnosed individuals will still need to isolate.
To accompany the plan revised social distancing guidelines have been issued.
Over time, social contact will be made less infectious by:
- making such contact safer (including by redesigning public and work spaces, and those with symptoms self-isolating) to reduce the chance of infection per contact;
- reducing infected people's social contact by using testing, tracing and monitoring of the infection to better focus restrictions according to risk; and
- stopping hotspots developing by detecting infection outbreaks at a more localised level and rapidly intervening with targeted measures.
Protecting the clinically vulnerable
- Some people are more clinically vulnerable to COVID-19 than others. These include those aged over 70, those with specific chronic pre-existing conditions and pregnant women. These clinically vulnerable people should continue to take particular care to minimise contact with others outside their households, but do not need to be shielded.
- Those in the clinically extremely vulnerable group are strongly advised to stay at home at all times and avoid any face-to-face contact; this is called ‘shielding’. It means not leaving the house or attending gatherings at all, with very limited exceptions.
There is no easy or quick solution. Only the development of a vaccine or effective drugs can reliably control this epidemic and reduce mortality without some form of social distancing or contact tracing in place.
|
European Bioinformatics Institute (EMBL-EBI) - COVID-19 Data Portal
18 April 2020 |
European Bioinformatics Institute (EMBL-EBI) has launched a COVID-19 Data Portal to facilitate data sharing and analysis, and to accelerate coronavirus research. The portal provides a ready means to share data and access research and findings.
|
International Long Term Care Policy Network - Mortality associated with COVID-19 outbreaks in care homes: early international evidence
12 April 2020 |
The International Long Term Care Policy Network at the London School of Economics and Political Science have published Mortality associated with COVID-19 outbreaks in care homes: early international evidence to examine deaths from COVID-19 in non-acute residential and nursing facilities that house people with some form of long-term care need.
Given the lack of consistent testing, it appears that the best way to estimate the mortality impact of COVID-19 in care homes, in the long term, will be by comparing mortality data from the period of the pandemic to mortality in previous years at the same time of the year.
In the mean time this report summarises information from epidemiological studies, official estimates and news reports.
Key findings from the study include ...
- Data from 3 epidemiological studies in the United States shows that as many as half of people with COVID-19 infections in care homes were asymptomatic (or pre-symptomatic) at the time of testing
- Data from 5 European countries suggests that care home residents accounted for between 42% and 57% of all deaths related to COVID-19.
Epidemiological studies carried out in the USA have attributed the spread of the disease in care homes to ...
- Staff who worked while symptomatic
- Staff who worked in more than one facility
- Inadequate familiarity with and adherence to Personal Protection Equipment (PPE) guidance
- Challenges to implementing proper infection control practices
- Delayed recognition of access due to low index of suspicion
- Limited availability of testing
- Difficulty identifying persons with COVID-19 on the basis of signs and symptoms alone
Across the 5 European countries, the percentage of COVID-19 death observed in care homes were ...
- Belgium - 42%
- France - 45%
- Italy - 53%
- Ireland - 54%
- Spain - 57%
Due to differences in testing availabilities and policies, and to different approaches to recording deaths, international comparisons are difficult This report will be updated as new information and data becomes available.
|
Coronavirus - COVID-19
March 2020 |
Although older people are no more likely to catch the coronavirus, COVID-19, than anyone else, the disease may have a more damaging effect in older age because the greater prevalence of underlying health conditions and a weaker immune system may lead to lower levels of resilience.
UK government sources recommend regular hand washing with soap and hot water for at least 20 seconds, to help reduce the spread of the infection, together with initial self-isolation at home for anyone who thinks they may have been infected.
A number of sources provide help and advice for older people ...
|
United for All Ages - Together in the 2020s
7 January 2020 |
United for All Ages has launched Together in the 2020s, a report which brings together 'twenty ideas for creating a Britain for all ages by 2030'.
The report outlines why a Britain for all ages is needed, then goes on to look at action for all ages in the community,in social and economic policy, and in culture media and sport.
It claims that Britain is one of the most age-segregated countries in the world.
Among the twenty ideas listed are -
- Ending ageism; Policies for all ages; A national positive ageing strategy; Designing a new 'twin economy';
- Legislating for the long term; A department for connection; An intergenerational curriculum; A bond for all ages
- Care homes as community hubs; Centres for all ages; Schools as community spaces; Streets for play;
- Intergenerational living; Homesharing; Training and learning together; Community planning by and for all ages;
- Online mentoring; Sport for life; Co-producing social innovation; A national day of unity.
|
House of Lords Science and Technology Committee - Inquiry into Ageing: Science, Technology and Healthy Living
25 July 2019 |
The House of Lords Science and Technology Committee has launched an inquiry into Ageing: Science, Technology and Healthy Living.
The inquiry will seek to determine whether the Government's ambition to increase health span is achievable in principle, and which approaches may be most successful in practice.
The Committee has put out a call for evidence and is asking for written evidence to be received by Friday 20 September 2019. It will start taking oral evidence for the inquiry in October 2019.
The Committee invites submissions on ...
- The scientific understanding of the ageing process, and how these areas of research could lead to treatments for delaying or managing the negative effects of ageing
- Technologies that can improve health and wellbeing in old age, and technologies that can enable independent living in old age
- Opportunities for the UK to commercialise discoveries and innovations relating to healthier ageing
- The policy implications of a healthier older population
|
All Party Parliamentary Group (APPG) on Housing and Care for Older People - Rental housing for an ageing population
17 July 2019 |
The UK Parliament All Party Parliamentary Group on Housing and Care for Older People has published Rental housing for an ageing population looking at rental housing for older people, now and in the decades to come.
Today only 22% of those over 65 are tenants (private or social) but the number of private renters has doubled since 2000, and the inquiry concludes that there will be very significant demand for affordable rented homes for older people over the next 30 years. It estimates a need of an average of 38,000 homes a year for rent, of which at least 12,000 should be Extra Care or sheltered.
The report notes that ...
- The absence of lifetime security of tenure is unsettling
- The poor condition of some properties is particularly bad for the health and wellbeing of older people.
- The chances of securing necessary adaptations - from handrails to stairlifts - is much lower in the private rented sector (PRS) than in other tenures.
- Very significantly, rents which may be affordable when a tenant is in work can become too expensive when they are reliant on pension income.
The numbers of households in the private rented sector (PRS) headed by someone aged over 64 will more than treble over the next 25-30 years (from around 450,000 today to over 1,500,000 in 2046). Assuming rents grow in line with earnings, around half of these older households in the PRS will no longer be able to afford the rent they could manage before they retired.
|
The Pensions Policy Institute (PPI) - Understanding the Gender Pensions Gap
11 July 2019 |
The Pensions Policy Institute (PPI) has published Understanding the Gender Pensions Gap looking at the pension savings gap between men and women and the major contributing factors.
The report notes that women currently on average earn approximately 18% less compared to their male counterparts and, over an individual’s working life, the pay differential could contribute to a reduction of pension wealth of 28% of those approaching retirement.
Women with pensions are, however, more likely than men to have saved in a Defined Benefit (DB) pension arrangement, at least in part because a larger proportion of women working in the public sector, which generally provides a DB pension arrangement.
Key findings include...
- Women taking time away from work, generally to look after family, is the biggest factor in the women’s pension gap.
- Over a working life, differences in participation rates have a small impact on pension wealth by retirement.
- The State Pension gap has been cut by over 70% with the new State Pension.
- In their early 60s the median private pension wealth of women is one third of men’s private pension wealth.
- To draw the same pension income throughout their retirement, women would need to have saved around 5% - 7% more than men by retirement age to allow for living longer.
A policy targeted at people not in paid work could reduce the gender pension gap. This is because a greater proportion of women take time out compared to men. Policies such as the family carer top-up could therefore reduce the pensions gap.
|
House of Lords, Economic Affairs Committee - Social care funding: time to end a national scandal
4 July 2019 |
The UK Parliament House of Lords Economic Affairs Committee has published Social care funding: time to end a national scandal, which gathers evidence and makes proposals for the future funding of adult social care.
The report finds that 'Social care funding is unfair. People receive healthcare free at the point of use, but are expected to make a substantial personal contribution towards their social care. In addition, national funding for social care is distributed unequally across local authorities.'
To address unfairness in the system the Committee proposes 'bringing the entitlement for social care closer to the NHS by introducing free personal care, which would include help with washing, dressing or cooking.
Those in care homes would still pay for their accommodation and assistance with less critical needs like housework or shopping. Those receiving care in their own homes would not have to pay accommodation costs, which may encourage care users to seek essential help with personal care early.'
Additional funding for social care should come from national government which should raise the money largely from general taxation. The money should be distributed to local authorities according to a fair funding formula.
Key conclusions and recommendations of the report are ...
- The Government must increase funding by £8 billion to restore levels of quality and access to those observed in 2009/10.
- The Government should introduce a basic entitlement to publicly funded personal care for individuals with substantial and critical levels of need. Accommodation costs and the costs of other help and support should still be incurred by the individual.
- To avoid catastrophic accommodation costs, the Government should also explore a cap on accommodation costs.
- The Government should adopt a staged approach to providing the additional funding recommended by this report. It should immediately invest £8 billion in adult social care, then introduce free personal care over the next five years. Free personal care should be available universally by 2025/26.
- Additional funding should be provided as a government grant, distributed directly to local authorities according to an appropriate national funding formula which takes into account differences between local authorities in demand for care and ability to raise funds from local taxation.
- Funding social care should be approached in the same way as any other funding pressure. Social care should be funded largely from general taxation.
The model proposed would cost £7 billion per year, only £2 billion more than the Government’s 2017 "cap and floor" proposal.
|
Policy Exchange - What do we want from the next Prime Minister? A series of policy ideas for new leadership: Social Care
23 June 2019 |
Policy Exchange has published What do we want from the next Prime Minister? A series of policy ideas for new leadership including Social Care, which makes recommendations for the future administration and funding of social care.
In polling carried out for Policy Exchange, in June 2019, over two thirds - 69 per cent - of respondents said they most agreed with the idea that "social care should be funded like the NHS, free at the point of delivery and paid for through general taxation".
The report's recommendations include ...
- Complete the welfare state by covering the costs of complex long-term social care, so that no individual or family faces ruinous costs or has to lose their home.
- Ensure that, like health care on the NHS, complex long-term social care is available on the basis of need - largely free at the point of delivery.
- End the present means test for complex social care. The capital component of the test should be eliminated altogether and the means-testing charging regime should be changed into a limited co-payment regime of the order of £5,000 per person per year, means-tested on income.
- Carry out a review of the assessment criteria and the thresholds of the need for care to ensure that there is consistency of provision across the country.
The report notes that total public expenditure currently accounts for about 38% of GDP, of which health absorbs 7.5%, the state pension 4.5% and social care 1%. The proposal fully to fund complex long-term social care would involve additional spending of some £11bn, or around 0.5% of GDP, equivalent to 1.3% of total public spending.
|
Policy Exchange - 21st Century Social Care
21 May 2019 |
Policy Exchange has published 21st Century Social care a report to identify "What’s wrong with social care and how we can fix it".
This politically oriented research paper explores the nature and extent of the problems affecting the provision of social care in the UK.
The report suggests that 'The institutional relationship between health and social care should be reviewed to assess whether social care should remain the responsibility of local authorities, given their other responsibilities and the changes being made to the local authority grant regime.'
and that 'There should be additional funding in the Government’s comprehensive spending reviews to remedy the long-standing neglect of social care that is gradually making the sector unviable'.
The report recommends ...
- Like health care, complex long-term social care in England should be available on the basis of need - largely free at the point of delivery.
- The present income and capital means test for complex social care should be ended. The capital component of the test should be eliminated and the means-tested charging regime should be changed into a limited co-payment regime of the order of £5,000 per person per year means-tested on income.
- The new co-payment regime should be constructed so that no present user pays more than they pay under the current means-testing arrangements and all users of the service face a co-payment no greater that £5,000. This would not preclude additional private payments for extra services.
- As a basis for consultation, the starting point for the co-payment should be around one and a half times average annual pensioner income which is approximately £27,000.
- This proposal would mean that care would be largely freely provided in people’s own homes, in residential care settings such as care homes and nursing homes and it would include what are described as 'hotel costs'.
The report also suggests that 'The NHS should be encouraged to work with the UK’s HealthTech sector, in areas like AI and robotics that could lead to improvements in the delivery of social care.'
|
Centre for Policy Studies - Fixing the Care Crisis
29 April 2019 |
The Centre for Policy Studies has published Fixing the Care Crisis, a report written by Damian Green MP, former first secretary of state in the Conservative government.
The report, which addresses how social care in older age should be paid for, notes the current lack of a political consensus and how political capital had been made out of previous proposals from both the Labour and the Conservative parties.
The report suggests that social care funding should be based on four principles...
- It must provide more money for social care and ensure it is spent wisely.
- The system must be fair across generations and medical conditions, and to those who have saved.
- The system must increase the supply of reasonably priced care options and retirement housing.
- The system should aim to secure public and cross-party consensus.
Damian Green suggests a model based on the pension system, with the state providing a universal care entitlement which could then be topped up with private support, for those who want it, via a Care Supplement. The scheme would be nationally funded.
It is estimated that this would cost an additional £2.75 billion per year which might be funded by taxing the winter fuel allowance and a 1% surcharge on National Insurance payments for the over 50s.
|
Centre for Ageing Better - The State of Ageing in 2019
13 March 2019 |
The Centre for Ageing Better has launched The State of Ageing in 2019, a report which gives a snapshot of ageing in the UK, today and in the future.
The report focuses on four main areas: work and finances; housing; health and communities.
Using data from existing sources, the report makes the following key points...
- Demography: In less than 20 years, the number of people aged 65 and over in the UK will increase by 44%, meaning that by 2037, one in four of the population will be over 65.
- Healthy life expectancy: Men at age 65 in the UK can expect to live about half the remainder of their life without disability - ten years of their 19 years. For women, the picture is worse - only ten years of their extra 21 years is spent without disability on average.
- Chronic health conditions: Nearly a quarter (23%) of people aged 50-64 manage three or more chronic health conditions. Compared to the wealthiest quintile, the poorest quintile of men aged 50 and over are 3x more likely to have chronic heart disease, 2x more likely to have Type 2 diabetes and 2x more likely to have arthritis.
- Life satisfaction: Life satisfaction peaks between 70 and 74, with this age group scoring on average nearly eight out of ten in response to the question: ‘How satisfied are you with your life nowadays?’
- Obesity: Levels of obesity are high amongst those approaching later life, and across all wealth groups in this cohort, though poorer people are more likely to be overweight or obese. More than 7 in 10 people aged 45 to 64 in England are either overweight or obese.
- Going out: A quarter (24%) of 55-59 year olds who don’t go out socially cite financial reasons, and one in ten 50-59 year olds cites caring responsibilities.
- Homes: Millions of UK homes are unsuitable for people with a disability or reduced mobility, with many being so hazardous and poorly-maintained that they pose a risk to the safety of their occupants. Just 7% of homes meet basic accessibility standards, and 1.3 million people aged 55 and over live in homes that pose a serious threat to health and safety.
- Work: The UK has 10.4 million workers aged 50 and over, an increase of 2.4 million in ten years. Nearly a third (3.3 million) of 50-64 year olds, more than the population of Wales, are not in work. A million people between 50 and state pension age are out of work prematurely, despite wanting a job, and poorer people are more likely to leave work due to ill-health.
|
Acas - Age discrimination: key points for the workplace
28 February 2019 |
Acas has published an advisory report Age discrimination: key points for the workplace, together with factsheets Age discrimination ten obligations for employers and Age discrimination top ten myths , outlining the legal and practical framework for dealing with ageism and age discrimination in the workplace in the UK.
Age is one of the nine 'protected characteristics' within the Equality Act 2010. In general, an employee is protected against discrimination because of age.
The Acas website linked to the report, outlines key areas where age discrimination may happen including: Recruitment; Training and promotion; Performance management; Managing under-performance; and Retirement.
For example, in relation to retirement the report reminds employers that: An employer must not treat an employee detrimentally because they are thinking about retiring or could already take their work pension or State pension nor should it change an employee's employment contract once they take any pension. Most employees now have the right to decide at what age they will retire. There is no legal, standard or default retirement age.
|
Ipsos MORI / Centre for Ageing Better - The Perennials: The Future of Ageing
13 February 2019 |
Ipsos MORI, in partnership with The Centre for Ageing Better, has published a report The Perennials: The Future of Ageing which looks at ageism and attitudes to older age.
Britons are overwhelmingly negative about old age. Only three in ten (30%) agree that they are looking forward to old age, while more than double (68%) disagree. Only 38% agree that they expect to be fit and healthy in old age, compared to one in five (22%) who disagree.
 |
Britons worry about older age.Three in ten (31%) mention losing mobility as something that concerns them. Financial worries are also prevalent (29% mention not having enough money to live on). A quarter (26%) mention losing their memory. |
Great Britain is in the mid-range of countries in terms of residents feeling prepared for older age, with residents of some South and Central American countries, Mexico, Colombia and Brazil, feeling the most prepared and those from some former communist countries, Poland, the Czech Republic and Russia, feeling the least prepared.
Views about what we should do to prepare for old age, in particular by saving, do not always match actual preparations.
|
|
NHS England - The NHS Long Term Plan
7 January 2019 |
NHS England has published The NHS Long Term Plan, outlining its vision for the medium to long term future of the NHS in England.
The report recognises that a growing and ageing population will inevitably increase the number of people needing NHS care and the intensity of support they require.
The report notes that the funding settlement announced by the Prime Minister in June 2018 promised NHS England's revenue funding would grow by an average of 3.4% in real terms a year over the next five years delivering a real terms increase of £20.5 billion by 2023/24. It claims that this represents a step change on recent years, which have averaged 2.2%, and moves closer to returning to the NHS long-term average funding trend of 3.7% per year since 1948.
Much of the report is applicable to both 'adults and older adults'. Measures specifically related to older adults include...
- Supporting people to age well - 'People are now living far longer, but extra years of life are not always spent in good health. They are more likely to live with multiple long-term conditions, or live into old age with frailty or dementia, so that on average older men now spend 2.4 years and women spend three years with 'substantial' care needs.'
- Dementia - 'We will go further in improving the care we provide to people with dementia and delirium, whether they are in hospital or at home.' 'Over the past decade the NHS has successfully doubled the dementia diagnosis rate and halved the prescription of antipsychotic drugs.'
- Social care - 'Both the wellbeing of older people and the pressures on the NHS are also linked to how well social care is functioning. When agreeing the NHS' funding settlement the government therefore committed to ensure that adult social care funding is such that it does not impose any additional pressure on the NHS over the coming five years. That is the basis on which the demand, activity and funding in this Long Term Plan have been assessed.'
- Pneumonia - 'Pneumonia continues to place a huge burden on the NHS - improving our response will help to relieve the pressure, particularly during winter. Community-acquired pneumonia is a leading cause of admission to hospital, despite being avoidable in many cases. Pneumonia also disproportionally affects older people, with incidence doubling for those aged 85-95 compared with 65-69. For every degree drop in temperature below five degrees Celsius, there is a 10.5% increase in primary care respiratory consultations and a 0.8% increase in respiratory admissions.'
- Carers and caring - 'Carers will benefit from greater recognition and support. The latest Census found that 10% of the adult population has an unpaid caring role, equating to approximately 5.5 million people in England - around 1.4 million of whom provide upwards of 50 hours care per week. 17% of respondents to the GP patient survey identified themselves as carers. Many carers are themselves older people living with complex and multiple long-term conditions. We will improve how we identify unpaid carers, and strengthen support for them to address their individual health needs. We will do this through introducing best-practice Quality Markers for primary care that highlight best practice in carer identification and support.'
Other measures include a greater emphasis on prevention and integrated care.
- Prevention - The report outlines programmes to cut smoking and obesity and double enrolment in the NHS Type 2 Diabetes Prevention Programme.
- Integrated care - The report outlines actions to 'redesign healthcare so that people get the right care at the right time in the optimal care setting (for example, providing better support to people living in care homes to avoid emergency hospital admissions; providing better social care and community support to slow the development of older people's frailty; and fundamentally redesigning outpatient services so that both patients' time and specialists' expertise are used more appropriately).'
|
Centre for Ageing Better - Age-friendly and inclusive volunteering: Review of community contributions in later life
19 October 2018 |
The Centre for Ageing Better has published Age-friendly and inclusive volunteering - a review of community contributions in later life.
Making a contribution to our communities is good for us. It improves social connections, enhances our sense of purpose and self-esteem and as a result, increases life satisfaction, happiness and wellbeing.
The report confirms findings of earlier research that poorer and less healthy people in later life face barriers to contributing within formal organisations but this is less marked for informal volunteering. There are gaps in the representation of people from some Black, Asian and Minority Ethnic (BAME) communities in formal volunteering.
The report also confirms earlier findings that it is important that volunteering by older people is 'appreciated'. An 'age-friendly' approach includes efforts to ...
- recognise the value and contributions of older citizens
- ensure people with additional support needs are enabled to contribute
- ensure flexibility, making it easy for older people to start, stop and change their contribution
- building age-friendliness into funding proposals
An age-friendly approach to volunteering should be built-in at all levels, including by local authorities, commissioners, businesses and employers, major funders and leadership bodies.
|
Skills for care - The state of the adult social care sector and workforce in England
24 September 2018 |
Skills for Care have published The state of the adult social care sector and workforce in England, setting out the characteristics of the entire adult social care workforce in England including age, gender, ethnicity and specific job role information.
The report includes: Size of the sector and workforce and what it looks like ; Employment overview - full/part time status, zero hours contracts; Recruitment and retention information - experience in sector, role, source of recruitment; Pay rates; Care certificate, training and qualification information; Personal assistant estimates and workforce characteristics; Workforce forecasts up to 2035.
Key findings for adult social care include...
- A quarter of the workforce (25%) were on a zero-hours contract (335,000 jobs).
- The staff turnover rate was 30.7%, equivalent to around 390,000 leavers in the previous 12 months.
- Many of these leavers move to other roles within the sector as 67% of recruitment is from within adult social care.
- Adult social care has an experienced 'core' of workers. Workers had, on average, 8.2 years of experience in the sector.
- The vacancy rate was 8.0%, equivalent to around 110,000 vacancies at any given time. The majority of these vacancies (76,000) were care workers.
- A fifth of all workers (320,000 jobs) were aged over 55 years old.
- The majority (83%) of the adult social care workforce were British, 8% (104,000 jobs) had an EU nationality and 10% (130,000 jobs) a non-EU nationality.
- According to the Government’s 'EU Settlement Scheme: statement of intent' the rights of EU citizens living in the UK will not change until after 31st December 2020.
The NMDS-SC shows that 21% of workers with an EU nationality also already have British Citizenship and that 50% of EU workers arrived in the UK either in or prior to 2015, and therefore may have gained the five years continuous residency required for ‘Settled status’. The remaining 29% of EU workers will be eligible for ‘pre-settled status.
- Prior to the National Living Wage, care worker hourly rates increased by around 13p (1.9%) per year. The launch of the NLW saw the average hourly rate increase by 20p (2.7%) then by 39p (5.2%) in the following year.
|
Office for National Statistics (ONS) - Changing trends in mortality
7 August 2018 |
The Office for National Statistics (ONS) has published two related reports Changing trends in mortality: an international comparison: 2000 to 2016 and Changing trends in mortality: a cross-UK comparison: 1981 to 2016, which show that, for the first time since records began, there has been a slow down in improvements in life-expectancy, both at birth and at age 65, in the UK.
This slow down occurs in several countries, for both men and women, but is particularly noticeable in the UK and for the 65 to 79 age group and is more noticeable for women than for men.
"Improvements (decreases) in UK mortality rates - the number of deaths divided by the population - have been slowing since around 2011. Most notably there was a sharp increase in deaths in 2015, which led to the first reduction in UK life expectancy at birth of the 21st Century."
A more detailed analysis of mortality rates within the UK shows...
- Mortality rates have worsened among those aged 15 to 54 years since 2012 in the UK, this contrasts with children aged 0 to 14 years who are continuing to show improvements in mortality rates.
- The rise in mortality rates for people aged 90 years and over reflects increases in mortality rates for mental and behavioural disorders, such as dementia.
- At the country level, England and Wales have seen a greater slowdown in overall mortality improvements for males compared with Northern Ireland and Scotland.
- The slowdown in mortality improvements at the oldest ages is seen for males and females and across all four UK countries but patterns in mortality at the younger ages are more complex and vary by sex and between the UK countries.
The reports note that "As mortality rates for males in Northern Ireland and Scotland have traditionally been higher than in England and Wales they may have seen less of a slowdown in improvements because the gains made by males in England and Wales might not yet be fully realised in Scotland and Northern Ireland."
|
Centre for Ageing Better - Transforming Later Lives
31 July 2018 |
The Centre for Ageing Better has published an updated strategy document, Transforming Later Lives.
The document set out a new strategic vision for the Centre for Ageing Better, with a clearer focus on people approaching later life and at risk of missing out on a good later life. The strategy aims to make changes that mean that more people enter later life free from disability, financially secure, supported by friends and family and with a purpose.
The strategy outlines four priority goals ...
- Fulfilling work: 1 million more people aged 50-69 in fulfilling work by 2022.
- Safe and accessible homes: by 2030 there will be 1 million fewer homes defined as hazardous and half of all new homes will meet accessibility standards.
- Connected communities: By 2030, an increase in the proportion of people aged 50 and over who report they feel they belong to their neighbourhood.
- Healthy ageing: people to have five more years free of preventable disability and to reduce the gap between the richest and poorest people in disability-free life expectancy by 2035.
The revised startegy aims to 'start with the person', be 'bold and innovative', 'focus on impact', be 'open and collaborative and 'grounded in evidence'.
|
House of Commons Health and Social Care Committee and Housing, Communities and Local Government Committee - joint report - Long term funding of adult social care
27 June 2018 |
In advance of the government green paper, now scheduled to be published in Autumn 2018, the House of Commons Health and Social Care and Housing, Communities and Local Government Committees have published a joint report: Long-term funding of adult social care.
The report finds that, in its present state, the social care system is not fit to respond to current needs, let alone future needs predicted as a result of demographic trends.
The discussions about how to reform social care and how to raise the additional funding required, needs to be informed by the following framework:
Providing high quality care; Considering working age adults as well as older people; Ensuring fairness on the ‘who and how’ we pay for social care, including between the generations; Aspiring over time towards universal access to personal care free at the point of delivery; Risk pooling—protecting people from catastrophic costs, and protecting a greater portion of their savings and assets; ‘Earmarking’ of contributions to maintain public support.
The report supports the provision of social care free at the point of delivery as a long-term aspiration. In principle, the personal care element of social care should be delivered free to everyone who has the need for it, but accommodation costs should continue to be paid on a means-tested basis.
Given the scale of the additional funding likely to be needed, a combination of different, local and national, revenue-raising options will need to be employed:
- At local level: There should be a continuation for the foreseeable future of the existing local government revenue streams and in the medium term, there should be a reform of the council tax valuations and bands to bring them up-to-date.
- In the future, as other funding streams develop, the contribution from council tax and business rates to social care funding could reduce.
- At national level: an additional earmarked contribution, described as a ‘Social Care Premium’, should be introduced, to which employers would also contribute. This can either be as an addition to National Insurance, or through a separate mechanism similar to the German model.
- The funding derived from the Social Care Premium should be placed in an appropriately named and dedicated fund. The fund should be regularly audited and required to publish its spending and accounts.
- Those aged under 40 should be exempt from the Social Care Premium, and it should also be paid by those over the age of 65.
- The principle of having an earmarked fund that the public could see is for social care could be extended to funding of the NHS. In the long term this could be 'reimagined' as ‘National Health and Care Insurance’, promoting an integrated service.
- To remove the catastrophic cost of care for some people, and to spread the burden more fairly, the report recommends that an additional amount of Inheritance Tax should be levied on all estates above a certain threshold and capped at a percentage of the total value.
The report states that, to make progress on reform, a cross-party approach on reforming social care funding is now essential and suggests that a parliamentary commission offers the best way to make progress on this issue.
|
The Health Foundation and The Kings Fund - A fork in the road: Next steps for social care funding reform
18 May 2018 |
The Health Foundation and the Kings Fund have published A fork in the road: Next steps for social care funding reform outlining a number of models for the future funding of social care.
The report does not make recommendations but tries to identify the advantages and disadvantages, impact and consequences of adopting each option.
The options considered are ...
- maintaining the current system (at 2015/16 levels) and keeping pace with projected demand pressures until 2030/31
- restoring the system to the level of quality and access that existed in 2009/10
- introducing a ‘cap and floor’ model, similar to the Conservative Party proposals at the 2017 general election
- introducing free personal care (FPC), similar to the model in Scotland
The models indicate that, if adopted, and setting the cap of £75,000 and the floor of £100,000 for the cap and floor model, the four options will require £1.5bn, £8bn, £5bn and £7bn respectively in additional annual spending by 2020/21.
Retaining the current system would involve minimal disruption to the administrative system, compared with implementing a new model, and no transition costs.
Returning to the level of quality and access observed in 2009/10, while meeting demand pressures since then, would require much greater levels of investment.
The cap and floor model prioritises protecting people from having to sell all their assets or facing catastrophic lifetime care costs. While being more generous as a whole, this option creates ‘winners and losers’ - more people would receive state-funded residential care but fewer would receive funding for domiciliary care.
Free personal care for all older people with eligible needs would remove one of the systematic barriers to integration with health. While expensive, it is not more expensive than investing to restore access to levels seen in 2009/10.
|
Association of Directors of Public Health (ADHP) - A Life Course Approach to Public Health
18 May 2018 |
The Association of Directors of Public Health (ADHP)has published a series of four 'position papers': Best Start in Life; Living and Working Well; Healthy Ageing; and Health Inequalities - outlining its policy positions.
The policy position on healthy ageing incorporates a number of recommendations:
- Governments across the four nations should take a whole system approach to positive ageing that starts at the beginning of the life course
- Investment in public health must be increased. Cuts to public health budgets must be reversed.
- NHS England needs to ensure that prevention forms a key, mandatory and funded part of all Sustainability and Transformation Partnership and Integrated Care System plans
- Reform of the social care system is needed urgently to ensure a system that is safe and sustainable.
- A more strategic approach is needed to deliver appropriate housing provision for the ageing population.
- National and devolved governments and local authorities should look at future proofing transport systems while ensuring they are appropriate for the ageing population
- Employ more positive rhetoric when discussing ageing to avoid negative stereotyping around older people and their abilities.
- Work with businesses to look at how best to support the ageing workforce and support older adults to re-train and continue lifelong learning.
- Invest in prevention of modifiable risk factors to help to reduce cases of dementia.
- Effective integration of health and social care services and a whole system, place-based approach
- An asset-based approach to older people’s health and consider approaches that utilise resources in the community
- Co-production approaches to developing interventions for older people
- Targeted interventions around fuel poverty
- Local authorities should work with hospitals and the voluntary and community sector to tackle malnourishment of older people in the community.
The report emphasises that inequalities in later life can be the product of cumulative disadvantage over time and socioeconomic status in early life has a strong bearing on future health outcomes.
It advocates a whole system approach to supporting older adults through joint working between local authorities, health and community partners. It notes that further cuts in public health expenditure will have a negative effect on services for older people.
The report emphasises the importance of prevention: "Primary, secondary and tertiary prevention should be embedded throughout the life course to maximise the opportunity for independent healthy ageing and to reduce inequalities in later life. At the primary prevention level this means supporting health promoting behaviors starting with pre-birth and the early years and continuing throughout the life-course. At the secondary and tertiary levels, it means delivering initiatives to ensure older people are living as healthily as possible, are connected to their communities and can access services including screening, immunisation and health checks."
|
Foundations and Housing LIN - Housing - Getting People Home from Hospital
15 May 2018 |
Foundations and the Housing LIN have developed an interactive map highlighting examples of where housing organisations and services are, or have been actively supporting hospital discharges and helping to get people home.
The map also displays NHS England-reported data showing the number of delayed discharges of care from hospital arising from housing issues across England. Between January - December 2017, NHS hospital trusts reported over 110,000 days lost to the NHS due to delayed discharges from hospital arising from a housing or related issue.
The main groups affected by delayed transfers of care are older people, people with mental health problems, and people experiencing homelessness.
Further details are available on the Housing LIN website.
|
Communities and Local Government (CLG) Select Committee - Housing for older people
9 February 2018 |
The Communities and Local Government (CLG) Select Committee published a report Housing for older people.
Older people are diverse and their housing needs and options are varied, reflecting their age, tenure, geographical location, income, equity, health and individual preferences. This gives rise to a range of issues - from home maintenance, adaptations and repairs, to access to financial advice, and to housing supply.
The report makes a number of key recommendations ...
- The existing FirstStop Advice Service should be re-funded by the Government to provide an expanded national telephone advice service
- The coverage of Home Improvement Agencies (HIA) should be expanded so there is access to at least one HIA with a handyperson service in each local authority area.
- A range of measures to help older people overcome the barriers to moving home should be implemented
- The National Planning Policy Framework should be amended to emphasise the key importance of the provision of housing for older people
- To facilitate the delivery of new homes, specialist housing should be designated as a sub-category of the C2 planning classification, or be assigned a new use class.
- Councils should publish a strategy explaining how they intend to meet the housing needs of older people in their area
- All new homes should be built to the Category 2 Building Regulations standard so that they can meet the current and future needs of older people.
- The Government should accept the Law Commission’s code of practice
- The social care green paper should consider the range of housing for older people, in particular the potential for extra care housing to play a greater role in providing social care alongside home care and residential care.
|
UK Government - Announcement of a green paper on care and support for older people - Summer 2018
17 November 2017 |
Damian Green, First Secretary of State and Minister for the Cabinet Office, has announced a green paper on care and support for older people to be published by Summer 2018.
The green paper will set out plans for how the government proposes to improve care and support for older people. The government has promised to work with independent experts, stakeholders and users to shape the long-term reforms that will be proposed in the green paper.
A number of independent experts have been invited to provide advice, and support engagement, in advance of the green paper.The experts include Andrew Dilnot, former Chair of the Commission on the Funding of Care and Support.
The full expert panel is made up of...
- Caroline Abrahams - Charity Director of Age UK
- Dame Kate Barker - former Chair of the King’s Fund Commission on the Future of Health and Social Care in England
- Sir David Behan - Chief Executive of Care Quality Commission
- Dr Eileen Burns - President of the British Geriatrics Society
- Professor Paul Burstow - Chair of the Social Care Institute for Excellence
- Jules Constantinou - President-elect of the Institute and Faculty of Actuaries
- Sir Andrew Dilnot - former Chair of the Commission on the Funding of Care and Support
- Baroness Martha Lane Fox - Founder and Executive Chair of Doteveryone
- Mike Parish - Chief Executive of Care UK
- David Pearson - former President of the Association of Directors of Adult Social Services and Corporate Director for Social Care, Health and Public Protection at Nottinghamshire County Council
- Imelda Redmond - National Director of Healthwatch England
- Nigel Wilson - Chief Executive of Legal and General
There will also be a full public consultation following publication of the green paper
|
Institute for Public Policy Research and Independent Age - Saving Social Care - A fair funding settlement for the future
14 November 2017 |
The Institute for Public Policy Research (IPPR) and Independent Age have published Saving Social Care - A fair funding settlement for the future, looking at the future demand for, and funding of, social care in the UK.
The increased demand for social care, coupled with cuts in funding since the onset of austerity, are likely to lead to shortfall in social care funding of £2.7 billion by 2020/21 and £9.5 billion by 2030/31.
The report finds that reductions in benefits, including means testing winter fuel payments or removing the triple lock on pensions are regressive and unlikely to fill the funding gap.
Key findings include ...
- Adult Social Care funding has been cut by 17% since its peak in 2009/10, with severe consequences including a large increase in unmet need and increased reliance on unpaid carers.
- These pressures are likely to grow and, without a funding settlement, will lead to a funding gap of £9.5 billion by 2030/31.
- Solutions sought would need to be, sufficient, inter and intra-generationally fair, and politically achievable.
The report concludes that increased taxation in the form of, for example, increased National Insurance Contributions or Inheritance Tax, would be a sufficient and fair way to fill the funding gap, but may not be politically achievable.
|
Calouste Gulbenkian Foundation UK Branch and the Centre for Ageing Better - Transitions in Later Life - Insight and Evaluation Reports
5th October 2017 |
Calouste Gulbenkian Foundation and the Centre for Ageing Better have published an Evaluation Report and an Insights report from an evaluation of a series of courses designed to help older people approaching retirement.
In parallel, a YouGov survey was commissioned of more than 1,000 people across the UK who had retired in the last five years, and more than 1,000 who are anticipating retiring within the next five years.
Key findings of the survey include ...
- One in five (20%) of adults who had retired recently found retirement difficult. Although 30% of retirees had reduced hours in preparation for retirement , over one half (56%) didn't do anything in particular to help themselves prepare for the change in lifestyle. Nearly one in five (19%) said they wanted more advice or support - mainly on managing money (45%); emotional aspects (39%); maintain and improving health (33%); and how to spend time (30%).
- Around half (56%) of UK workers planning to retire in the next five years are looking forward to it. The main concerns are worry about managing money (41%); concern about feeling bored (33%); missing social connections from work (32%); losing a sense of purpose (24%); and being lonely in retirement (17%). Although 37% are planning to reduce working hours, 45% have made no arrangements.
- Women worry about retirement more than men and are more likely to get involved in the local community after retirement.
The evaluation report found that the courses, which had focussed on the psychological aspects of retirement, had resulted in improved attitudes and outlook in terms of: confidence and readiness for the future; resourcefulness; positive attitudes to ageing and the future; social connections and reduced loneliness; and a sense of purpose.
|
Local Government Association and Housing LIN - Housing our Ageing Population: Learning from councils meeting the housing needs of our ageing population
8 September 2017 |
The Local Government Association (LGA) and Housing LIN have published Housing our Ageing Population: Learning from councils meeting the housing needs of our ageing population which provides an overview of recent policy and practice developments and shows how local councils in England are addressing the housing needs of their ageing populations.
Using examples from Birmingham; Central Bedfordshire; Essex; Mansfield; Newcastle; North Somerset, Bristol Bath and North East Somerset; and Worcestersire councils, the report identifies the following key themes and lessons:
- Having a clear vision: promoting awareness and changing attitudes
Including: downsizing to well designed 'care ready' homes; releasing family homes back to the market; acheiving efficiencies in delivering personal home care in developments for older people.
- Planning for an ageing population
Using a mixture of demographic data, planning tools, local need plans, engaging with developers and older people and co-production
- Delivering and enabling new housing for older people across the public and private sectors
Disposing of public sector land provides an opportunity to allocate sites for older people's housing; encouraging and supporting private sector retirement housing development.
- Promoting and integrated approach to housing, care and health
Supporting older people to return to their homes after hopital care including practical assistance to reduce the likelihood of falls.
- Sustaining older people in mainstream housing
Commissioning and providing home improvement agency type services across council boundaries offers scope for economies of scale that can support and foster innovation in improving existing housing.
The report concludes that a renewed national and local effort to build more homes for older people needs to be intelligence led; enabled by local planning; collectively led by housing and health partners; embrace opportunities to increase supply; integrate housing, health and care strategies; successfully adapt existing housing; and fully inform older people of their options for their current and future housing needs
|
Institute for Fiscal Studies - Can't wait to get my pension
2 August 2017 |
The Institute for Fiscal Studies (IFS) have published Can't wait to get my pension: the effect of raising the female state pension age on on income, poverty and deprivation. Using a difference-in-differences methodology,the report estimates the impact of the changes in women's state pension age on women’s incomes, income poverty rates and measures of material deprivation.
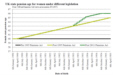 |
This paper estimates the impact of increasing the female state pension age in the UK from 60 to 63, between April 2010 and March 2016, on the incomes of women aged 60-62. It finds that, on average, household incomes were reduced by £32 per week, with an increase in employment income partially offsetting a larger fall in income from state benefits. |
After accounting for behavioural change, it estimates that the public finances were strengthened by £5.1 billion, of which £4.2 billion came from reduced benefit spending (net of tax, where applicable) and £0.9 billion from increased direct tax receipts elsewhere.
Women from lower-income households are found to have experienced a relatively greater cut to their net incomes, and the poverty rate among women aged 60-62 is found to have increased by 6.4ppts as a result of the state pension age rising from 60 to 63. The increases in poverty rates are greater among groups for whom income poverty is more prevalent: singles rather than those in couples; renters rather than owner-occupiers; and those with fewer, rather than more, years of formal education.
The report finds no evidence of any increase in the likelihood of women reporting being deprived of important material items, potentially suggesting that many affected families have smoothed their consumption, and avoided increased levels of deprivation, despite the large reduction in income caused by the reform.
|
|
Ipsos MORI - Unmet need for care
20 July 2017 |
Following secondary analysis of English Longitudinal Study of Ageing (ELSA) and Health Sorvey for England (HSE) data, carried out in collaboration with Age UK, Independent Age and NatCen, Ipsos MORI have published a final report - Unmet Need for Care exploring the unmet needs of older adults who live in their own homes. Both a full report and an Executive Summary are available.
The study confirmed previous research that unmet need for social care is widespread. The data from ELSA and HSE showed over half of older people with care needs had unmet need for support with at least some of their difficulties and this cut across all groups regardless of wealth, age or other socio-demographic factors.
In-depth interviews found that, while participants did not often report unmet need with basic activities of daily living, where they did not have support, carrying out these activities could take a disproportionate amount of time and lead to pain and exhaustion. Where support was available it was often precarious.
Secondary analysis showed that the only significant factors which predicted the development of care needs over a ten-year period were being younger and healthier at the start, living alone or being widowed and having difficulties with personal care rather than more general activities of daily living.
Older people find unmet need for social contact and mobility to be as important, if not more important than meeting basic needs of daily living. Links between unmet need and well-being are related to the pressures involved in coping day to day, associated loss of wider interests and mobility, and lack of social contact.
The study found that older people showed resilience and independence in meeting their needs and the challenges they faced. This was associated with positive well-being, even in the face of unmet need for support with particular tasks.
The responsibility for tackling unmet need for care lies not just with social care practitioners and providers but with wider services and society. This includes accessible and affordable or free public transport, being supported in maintaining hobbies or interests, and having control over housing and the ability to keep it warm and add adaptations when they needed them.
|
Institute of Health Equity - Marmot indicators 2017
18 July 2017 |
The Institute of Health Equity have released the Marmot indicators 2017, a set of indicators of health inequality.
The latest indicators show that the steady upward trend in life expectancy at birth and at age 65 ,for both men and women, which has been observed since 2000, has since 2010, begun to fall back.
The briefing notes that while Ischaemic heart disease remains the most common cause of death for all age groups from 45 to 84, from age 85+ Dementia and Alzheimers disease is the most common cause of death.
Between 2002 and 2015 there has been a 175% increase in dementia as a contributor to cause of death for women aged 85 and over and a 250% increase for men of the same age.
The report notes inequality in life expectancy both between and within individual boroughs. Kensington and Chelsea which has the highest life expectancy overall also has one of the highest levels of inequality in life expectancy within the borough.
|
Association of Directors of Adult Social Services (ADASS) - Budget Survey 2017
28 June 2017 |
The ADASS Budget Survey is an annual survey conducted by the Association of Directors of Adult Social Services (ADASS), and is sent to every Director of Adult Social Services (Directors) in 151 English local authorities.
The current survey points to a £1bn gap between the amount councils would need to spend to keep pace with demand and cost pressures and the funding available.
The survey found that the "negative consequences" of service cuts had already been felt on the frontline. Three quarters of directors reported care providers in their areas were in financial difficulty, 70% said providers were struggling to maintain quality services, and 74% said the NHS was under more pressure.
Over a quarter of directors (27%) also said that life for carers was worse, and 17% said the quality of life for people using social care services has deteriorated. A third said they faced a rise in legal challenges over social care last year and 38% expected a further increase in coming years.
Key findings include ...
- The proportion of council spending on adult social care is due to increase to 36.9% this year, compared with 35.6% in 2016-17
- The additional £2bn, over 3 years, goverment funding for Social Care, outlined in the March 8th 2017 Budget, will help close the funding gap facing adult social care, but councils still plan to make further savings of £824m this year
- Prevention - Increasing preventative services is now seen by directors as the most important way of realising savings, followed by better procurement practices and shifting care provision to cheaper settings. However, the spend on prevention had reduced in previous years and as budgets are cut further "it becomes harder for councils to manage the tension between prioritising statutory duties and investing in services that will prevent and reduce future needs". Spend on prevention forms 6.3% of budgets this year: this is both a decrease as a proportion of budget and a decrease in cash terms from the previous year.
- Delayed discharge - 16% of councils had received fines from the NHS for delayed discharges from hospital while a further 8% said the 'intention to fine' had been expressed.
Further savings of £824m, equating to 5% of net budgets, are planned in 2017/18. Total cumulative savings in adult social care since 2010 will amount to over £6bn by the end of March 2018.
|
Office for National Statistics - An overview of lifestyles and wider characteristics linked to Healthy Life Expectancy in England: June 2017
28 June 2017 |
The Office for National Statistics (ONS) has released a geographically-based analysis of Healthy Life Expectancy in England, An overview of lifestyles and wider characteristics linked to Healthy Life Expectancy in England: June 2017.
 |
In this analysis, average Healthy Life Expectancy (HLE)at birth is calculated for each Upper Tier Local Authority (UTLA) based on a subjective assessment of an individual's own health. HLE is then compared with a number of other potentially causative factors for that UTLA. |
On a regional basis, Healthy Life Expectancy is most strongly related to levels of preventable illness, followed by, in order, episode rates for alcohol related conditions, levels of physical activity, adherence to healthy eating guidelines, smoking prevalance and levels of obesity.
Areas with higher levels of unemployment and a higher proportion of routine and semi-routine occupations have lower levels of Healthy Life Expectancy as do areas with a lower proportion of people with qualifications at NQF level 4 and above.
|
|
Pensions Policy Institute - WHERL - The Wellbeing, Health, Retirement and the Lifecourse project
20 June 2017 |
Pensions Policy Institute (PPI) have published the final report from The Wellbeing, Health, Retirement and the Lifecourse project (WHERL), a joint project with King’s College London, University College London the University of Manchester, the University of Toronto, DWP and Age UK.
The WHERL project examined the lifelong drivers affecting the relationship between paid work in later life, health, wellbeing and retirement income, to assess the effect of policy initiatives such as the increases to the State Pension Age, removal of default retirement ages, and the Government’s ‘Fuller Working Lives’ and ‘Age Positive’ initiatives.
Key findings include...
- Work and retirement patterns are complex but older men (born 1920-49) are more likely than women to have experienced a longer history of full employment. A minority (8%) who are socio-economically advantaged however start work later in life and retire early. Cohort analysis reveals that, for men, working full-time throughout the life course is becoming less common.
- A large proportion (57% of men born 1932-45 and 46% of women born 1937-50) were not in the labour market in the decade around (5 years before and after) state pension age.
- Retirement reversal is common with one quarter of older adults returning to paid work within 15 years of 'retiring'.
- The ability to work past state pension age depends on health, especially for men, while health at state pension age depends on labour market and family experiences earlier in the lifecourse. After controlling for these factors, there are no health benefits or disadvatages of working past State Pension Age.
- Women approaching retirement have much more varied lifecourses than men and have accumulated far less pension. Around 73% of women in their 70s in 2017 had long breaks from paid work (10+ years)
There is a correlation between more advantageous characteristics (such as higher levels of education, good health, and higher household income) and working beyond State Pension Age. In contrast, those who leave the labour market at a very early age (around 49) often exhibit lower levels of education and health. This suggests that those who could perhaps benefit the most from working beyond State Pension Age in order to increase their income in retirement, may be unable to do so either as a result of poor health or limited access to appropriate employment opportunities.
|
Older People in the Election Manifestos - Centre for Policy on Ageing
23 May 2017 |
The Centre for Policy on Ageing has published Older people in the manifestos, a document of extracts from the manifestos to summarise what the three main parties said about older people, in their manifestos, in the 2017 UK general election.
This document provides extracts from those aspects of the three main manifestos in England, the Conservatives, Labour and Liberal Democrats, that are of particular relevance to older people, either because they address older people directly by considering our ageing society or inter-generational issues or are topics of particular relevance such as pensions, older-age benefits and health and social care.
The full manifesto documents for the Conservatives, Labour and the Liberal Democrats are also available.
|
Independent Age - Care home performance across England, March 2017
11 April 2017 |
Independent Age has published Care home performance across England, March 2017, a regional review, based on CQC inspection data.
Using data from individual local authorites the report generates colour coded regional maps with, for homes rated ‘Inadequate’ or ‘Requires Improvement’, areas with up to 20% coloured green, more than 20% and up to 30% yellow, more than 30% and up to 40% orange and more than 40% coloured red.
 |
The analysis shows that that the North West is a particular area of concern, with a high proportion of care homes that are not performing well according to the CQC. In the North West, as many as one in three care homes fall into the Inadequate or Requires Improvement categories, as compared to just one in five in London and the East of England.
A more detailed break-down within regions shows that authorities with a higher proportion of poorly performing care homes are often clustered together in areas of urban deprivation or industrial decline, but that is not universally the case.
|
|
House of Commons: Communities and Local Government Committee - Adult social care
27 March 2017 |
The UK Parliament House of Commons, Communities and Local Government Committee has published a report on Adult Social Care. An executive summary and the full report are both available.
The report states that the Government needs to urgently review how social care is funded in the long term and address serious threats to social care provision. Inadequate funding very seriously affects the quantity and quality of adult social care provision, impacting on those receiving care, the NHS, care staff, carers and providers.
The report sets out a number of recommendations relating to the monitoring of care services, care commissioning, and the care workforce and suggests that the forthcoming green paper on social care should:
- look at a range of all possible revenue options including hypothecating national taxation (e.g. income tax or a compulsory new social insurance scheme) and age-related expenditure (e.g state pension, winter fuel allowance)
- consider the wide range of uses for which social care funding is required, including care and support, early intervention and prevention, and the training and development of care staff
The report finds that funding constraints are leading to councils providing care and support to fewer people, concentrating it on those with the highest needs, with care becoming the minimum required for a person to get through the day. It concludes that gaps in funding have led to a deterioration in the overall quality of care and that this is likely to continue and reports the already well known fact that care providers are relying on their privately paying clients to subsidise local authority funded clients by paying higher costs for the same care.
|
John Cridland CBE - Independent Review of the State Pension Age: Smoothing the Transition
23 March 2017 |
As part of a review of the state pension age after 2028, John Cridland CBE has published his final report - Independent Review of the State Pension Age: Smoothing the Transition.
The analysis features Baby Boomers (born 1945-65), Generation X (born 1966-1979) and Generation Y (born 1980-2000) and looks at changing longevity, affordability, inter and intra-generational fairness and the effects on particular groups, setting the State Pension age and smoothing the transition.
The report estimates that the cost of the state pension will rise from 5.2% of GDP in 2016/17 to 6.2% in 2036/37.
The report suggests that individuals need at least ten year's notice of state pension changes and such changes should be limited to once per decade.
Recommendations include ...
- State Pension age across the UK should increase to reflect changes in life expectancy.
- State Pension age should rise to age 68 over a two year period starting in 2037 and ending in 2039 but, based on current data, State Pension age should not increase by more than one year in any ten year period.
- If further savings are needed, pensions should be uprated solely in line with earnings and, in the next parliament, the 'triple lock' should be abolished.
- Some of the funding released by changes in State Pension age and other aspects of the State Pension system should be re-invested to support disadvantaged groups.
- To help support people working past state pension age, people reliant on State Pension should be given some of the same flexibilities as those who have private pension provision.
- There should be a system of Statutory Carers' Leave for people with caring responsibilities.
The report also encouraged the Automatic Enrolment Review to look at improved pension coverage for women and the growing number of self-employed people.
|
Department for Work and Pensions and Government Actuary's Department - Periodic review of rules about State Pension age
23 March 2017 |
The Department for Work and Pensions and Government Actuary's Department have published the Periodic review of rules about State Pension age: report by the Government Actuary.
 |
This report aims to determine pension age rules that would be required for an average person to spend a specified proportion of their adult life (aged 20+) eligible to receive the state pension.
The report looks at the period from 2028 to 2064 and makes mortality assumptions based on ONS 2014 principal population projections. Two scenarios are considered, one third (33.3%) of adult life and 32% of adult life.
|
For an individual born after 6th April 1986, the state pension age would need to rise from 68 (as currently set) to 69 to achieve the 33.3% scenario or 70 to achieve 32%.
|
Office for National Statistics - Changes in the value and division of unpaid volunteering in the UK: 2000 to 2015
16 March 2017 |
The Office for National Statistics (ONS) has released the latest statistics of unpaid volunteering in the UK, Changes in the value and division of unpaid volunteering in the UK: 2000 to 2015.
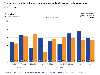 |
In 2000, older people, aged 65 and over, followed by those aged 55-64, spent more time volunteering than any other age group. By 2015 that was no longer the case with over 65s in particular, spending much less time volunteering and being overtaken by 16-24 year olds.
Retired people saw a fall in their average time spent volunteering, from 21 minutes per day in 2000 to 15 minutes per day in 2015.
|
|
Office for National Statistics - Overview of the UK population: March 2017
03 March 2017 |
The Office for National Statistics (ONS) has released the latest UK population estimates, Overview of the UK population: March 2017.
The UK population grew to an estimated 65.1 million in 2015.
 |
The proportion of the population that is aged 65 years or older is growing. It has increased from 14.1% of the population in 1975 to 17.8% in 2015. It is projected to continue to grow to nearly a quarter of the population by 2045.
Meanwhile the grandchildren of the post second world war baby boomer generation are creating a boom in the number of primary school aged children.
|
|
Nuffield Trust - Shifting the balance of care: Great expectations
02 March 2017 |
The Nuffield Trust have published a new report Shifting the balance of care: Great expectations, a review of Sustainability and Transformation Plans (STPs) and related literature on moving care out of hospital.
The NHS is facing a £22 billion gap in its finances by 2020/21 and it is hoped that, moving care out of hospital will deliver the ‘triple aim’ of improving population health and the quality of patient care, while reducing costs.
The report groups its evidence into: Changes in the elective care pathway; Changes in the urgent and emergency care pathway; Time-limited initiatives aimed at avoiding admission or facilitating discharge from hospital; Managing ‘at risk’ populations including end-of-life care and support for people in nursing homes; and Support for patients to care for themselves and access community resources.
The most effective interventions overall, in term of reducing hospital activity and cost. appear to be ...
- Improved GP access to specialist expertise
- Ambulance/paramedic triage to the community
- Condition-specific rehabilitation
- Additional clinical support to people in nursing and care homes
- Improved end-of-life care in the community
- Remote monitoring of people with certain long-term conditions
- Support for self-care
...however the parallel aims of improving population health and the quality of patient care seem to have fallen by the wayside.
|
Office for National Statistics - Most common age at death, by socio-economic position in England and Wales
21 February 2017 |
The Office for National Statistics (ONS) has released a review of mortality in England and Wales, Most common age at death, by socio-economic position in England and Wales: a 30 years comparison.
The review highlights improvements in mortality between 1982-86 and 2007-11, as well as inequalities in mortality between 'Higher Managerial and Professional' and 'Routine' occupations.
 |
In England and Wales for the period 2007 to 2011, the most common age at death was 85.6 years for men and 88.3 years for women, an increase of 8.2 years and 3.8 years respectively since 1982 to 1986.
In 2007 to 2011, the most common age at death for the men and women classified to the higher managerial and professional occupations was 86.8 years and 89.4 years, which is 2.4 years and 2.7 years higher than the men and women classified to the routine occupations.
|
|
Local Government Association and FaithAction - Working with faith groups to promote health and wellbeing
17 February 2017 |
Local Government Association and FaithAction have published Working with faith groups to promote health and wellbeing, a report indicating how local government can benefit from working with faith based groups and organisations.
The report suggests that there is a growing body of research which shows how faith groups can have a positive impact on both the health of their members and wider communities. Faith groups can generally be considered as part of the voluntary and community sector (VCS).
Some of the main ways in which faith groups can have a positive impact on health and wellbeing include ...
- support for ethnic groups who face health inequalities or are at greater risk of developing specific health problems
- social action to improve the lives of people who face problems such as poverty or homelessness
- articulating the health needs of their communities.
- In addition, regular involvement in faith activity is linked with greater health and wellbeing for faith members.
While faith and ethnicity are not identical, they are often closely linked and the report suggests that faith based organisations can focus on the most prevalent health problems associate with particular ethnicities, for example South Asians are at increased risk of cardiovascular disease and TYPE 2 diabetes.
The report lists a number of examples of faith based organisations oriented towards improving health and wellbeing and raises a number of questions for public health to consider when working with faith groups.
|
Nuffield Trust, The Health Foundation and The Kings Fund - The Autumn Statement: Joint statement on health and social care
08 November 2016 |
The Nuffield Trust, The Health Foundation and The Kings Fund have issued The Autumn Statement - Joint statement on health and social care outlining the urgent need to address the critical state of social care in England.
Research carried out by the organisations has found that the system is increasingly struggling to meet the needs of older people, their families and carers,
The publicly funded social care system faces the prospect of a £1.9 billion funding gap in 2017. It is therefore suggested that the government should bring forward the additional funding that will be provided through the Better Care Fund.
Key points include ...
- In 2015/16, the Department of Health exceeded its total departmental expenditure limit (TDEL) by £149 million. This overspend was largely a result of a net deficit for NHS trusts of £2.5 billion.
- Total health spending in England will rise by £4.2 billion in real terms between 2015/16 and 2020/21. Looked at over the whole of this parliament, this will result in a real-terms increase of on average 1.1 per cent a year, almost identical to the rate of increase over the last parliament.
- Real-terms funding increases of 0 per cent in 2018/19 and 0.3 per cent in 2019/20 are inadequate and will not be enough to maintain standards of care, meet rising demand from patients and deliver the transformation in services outlined in the NHS five year forward view.
- Public health spending will fall by at least £600 million in real terms by 2020/21, on top of £200 million cut from the budget in 2015/16. This is already affecting spending on services such as smoking cessation and sexual health services.
- Overall, NHS spending in the United Kingdom as a proportion of GDP is projected to fall to 6.9 per cent by 2020/21.
- After six years of unprecedented budget reductions, the number of people aged over 65 accessing publicly funded social care has fallen by at least 26 per cent, imposing significant human and financial costs on older people, their families and carers, and exacerbating pressures on the NHS.
Despite the ageing population and rising demand for services, UK public spending on social care is set to fall back to less than 1 per cent of GDP by the end of this parliament, leaving thousands more older and disabled people without access to services.
|
Independent Review of the State Pension age - Interim Report
13 October 2016 |
John Cridland,acting on behalf of DWP, is carrying out an Independent Review of the State Pension age, and has produced an Interim Report to which responses are requested by 31st December 2016.
The review is forward looking and only 'takes note' of the existing arrangements to April 2028 which are already law. The report defines three generations that feature throughout the analysis: Baby Boomers (born 1945-65), Generation X (born 1966-1979) and Generation Y (born 1980-2000).
The report looks at three aspects - Affordability, Fairness and Fuller Working Lives. Affordability which is a relative and 'political' concept, is not fully defined but, in the report, is measured in terms of changes in the dependency ratio, and spending as a proportion of GDP.
In assessing fairness, the report focuses on on intergenerational fairness - whether outcomes are fair between each generation of pensioners - and intragenerational fairness - whether outcomes are fair within each generation of pensioners now and in the future. Supporting Fuller Working Lives is seen as key to supporting any changes in State Pension age by giving people the opportunity to work longer.
The review looks a groups who are particularly seriously impacted including ...
- Carers - around 1 in 10 adults have some caring responsibilities and some have suggested this is likely to increase in the future. Carers are more likely to have breaks in their work history, leading to an estimated gap between carers’ and non-carers’ median income in retirement of 4%.
- People with disabilities - who may also face challenges in building up a private pension, particularly for those who are disabled from a young age. For non-disabled people, projected median income in the first year of retirement is around 7% higher than for those with disabilities. Stakeholders report that individuals working in certain professions have a higher risk of having to drop out of work early due to ill health or disability.
- Self-employed people - a diverse group with hugely different incomes and employment experiences. There is evidence to suggest that there is a downwards trend of self-employed people saving into a private pension, which means this group could become over-reliant on State Pension in retirement.
Responses should be emailed to spa.review@dwp.gsi.gov.uk
|
Ready for Ageing Alliance - Still not Ready for Ageing
16 September 2016 |
The Ready for Ageing Alliance, in a review of their manifesto called Still not Ready for Ageing conclude that Government action on tackling the challenges and maximising the opportunities of ageing has stalled and far from seeing sustained progress over the past few years, society is seemingly going into "reverse gear" in some respects.
The review agrees with the Government Office for Science, July 2016, Foresight report "Future of an Ageing Population" which stated that government will require a co-ordinated response between departments that reflects the robust evidence for the inter-connectedness of policies affected by ageing.
The Ready for Ageing Alliance argues that we are a long way from achieving this ...
- Savings levels remain far too low and, without significant increases, future generations of older people will find themselves poorer than today’s pensioners.
- Real wage growth is low, meaning that the incomes of most younger people do not allow them to save more.
- Social Care funding reform has received little discussion since plans for its reform were shelved and the funding gap in social care, which grows by the day, is a disaster for older people today and tomorrow
- Health and care face major staffing shortages over the short and medium term and unless this reality is properly gripped now we are storing up even bigger problems for the future
- Our economy loses billions due to the underemployment of older people who would prefer to keep working but who can’t because of ageism and/or a shortage of flexible working opportunities
- Isolation and loneliness remain blights on our society, with too little progress in ensuring communities are equipped to help us live independently for longer.
- We have a huge undersupply of retirement housing and new mainstream housing is not meeting the needs of older people today or tomorrow.
The Ready for Ageing Alliance calls for - An urgent focus on the crisis in social care with the aim of achieving a sustainable long term financial settlement which ensures people's care needs are met; The planned review into auto-enrolment to be extended to look broadly at how to increase savings and ensure today's young people - our future pensioners - can realise an adequate income when they reach later life; The creation of a permanent commission on Demographic Change which would focus on making progress in responding to our changing society; and A single point of contact in Government responsible for leading and responding to the challenges and opportunities of ageing set out by the Chief Scientist.
|
The Kings Fund and Nuffield Trust - Social care for older people: Home truths
15 September 2016 |
The Kings Fund and Nuffield Trust have jointly published Social care for older people: Home truths, a report looking at the current state of social care services for older people in England, through a combination of national data and interviews with local authorities, NHS and private providers, Healthwatch and other groups.
The report paints a bleak picture of social care providers under pressure, struggling to retain staff, maintain quality and stay in business; Local authorities making difficult choices about where to make cuts; A complex set of causes of delays in discharging older people from hospital; and A voluntary sector keeping services going when funding is curtailed.
Key findings include ...
- Social care for older people is under massive pressure; increasing numbers of people are not receiving the help they need, which in turn puts a strain on carers
- Access to care depends increasingly on what people can afford - and where they live - rather than on what they need.
- Under-investment in primary and community NHS services is undermining the policy objective of keeping people independent and out of residential care
- The Care Act 2014 has created new demands and expectations but funding has not kept pace. Local authorities have little room to make further savings, and most will soon be unable to meet basic statutory duties.
The report says that policy makers will need to ...
- achieve more with fewer resources - for example, through better commissioning and integrated care, while recognising that these initiatives will not be enough to close the funding gap
- establish a more explicit policy framework, which makes it clear that primary responsibility for funding care sits with individuals and families
- reform the long-term funding of social care because reliance on additional private funding is unlikely to be sufficient or equitable.
|
Government Office for Science - Foresight - Future of an Ageing Population
7 July 2016 |
The Government Office for Science, as part of its Foresight programme, has published Future of an Ageing Population, a comprehensive review of the implications of population ageing in the UK.
The report indicates that, overall, mainly as a result of the ageing population, public expenditure will need to rise from 33.6% of GDP in 2019/20 to 37.8% by 2064/65.
Key findings include ...
- Working lives: The proportion of the working age population aged between 50 and the state pension age (SPA) will increase from 26% in 2012 to 35% in 2050. Priority areas include:Supporting the ageing population to lead fuller and longer working lives; Adaptations to the workplace including addressing negative attitudes to older workers and health needs; improving workplace design, encouraging access to new technologies, and adaptation of human resources policies and working practices; and Ensuring individuals re-skill throughout their life time.
- Lifelong learning: Lifelong learning has a number of benefits alongside those related to work. Many kinds of learning boost mental capital, which in turn increases individual resilience in later life. There are positive effects of learning on both physical and mental health, improving wellbeing and reducing pressures on family and community resources and services.
Priorities include: Addressing falling participation in lifelong education and training; Addressing barriers to later life learning; and a specific focus on technological and financial skills through life.
- Housing and neighbourhoods: By 2037 there are projected to be 1.42 million more households headed by someone aged 85 or over. Priorities include: Ensuring there is appropriate housing; Thinking ‘beyond the building’ to include the neighbourhood and community; Preparing for the impact of variable home ownership rates - Housing can be a financial asset, providing financial security, a source of funding for care and being passed on as an inheritance. However, housing can also represent a significant financial burden if individuals still have large mortgages or rent when they enter retirement.
- A central role for families: Families are a central component of the drivers and implications of population ageing. Priorities include: Understanding the impact of increasingly diverse family types on policy, especially adult social care; Responding to smaller and more ‘vertical’ family units; Considering policies’ effects on the whole life course and understanding the dependencies between generations.
- Health and care systems: Ageing will increase the total amount of ill-health and disability in the population. Priorities include: Adapting health and care systems to meet changing demand; Supporting family and other unpaid carers; Capitalising on the opportunities from new technologies.
- Social, physical and technological connectivity: Connectivity - the ability to use technology, access services, travel easily and socialise - will be particularly important as the population ages. Priorities include: Responding to the transport needs of different age groups; Successfully designing the built environment; and Addressing barriers to technology use.
- A coherent response to ageing: The following principles will help to ensure a coherent response to ageing: The future success and resilience of the UK will be determined in a large part by its ageing population; Issues cannot be addressed in silos; Most domestic policy areas will be affected by the ageing population; Factors throughout an individual’s lifetime affect how they age; and Regional variation must be understood.
The ageing population presents real opportunities. However, there are challenges, and ignoring these could undermine the potential benefits of living longer.
The Centre for Policy on Ageing carried out a series of twelve international case studies on behalf of the programme.
|
Independent Age - The overlooked over-75s: Poverty among the ‘Silent Generation’who lived through the Second World War
16 May 2016 |
The Independent Age report The overlooked over-75s: Poverty among the ‘Silent Generation’who lived through the Second World War provides an analysis of the financial circumstances of older people with a focus on those people aged 75 and over. The report is based on an analysis of data from the Family Resources Survey (FRS).
The analysis shows that those aged 75 and over have lower incomes, on average, than younger adults. Many are living in poverty and are unlikely to see significant increases in their income during their lifetime.
Key findings include ...
- Older pensioners’ incomes are on average £59 a week lower than younger pensioners, and £112 a week lower than working age adults, or almost £6,000 a year
- One fifth of those aged 75 and over are living below the poverty line, including a quarter of single women aged 75 and over
- Over 75s are twice as likely as under 75s to have been in poverty persistently for the last four years.
- Among the over 75s, women, single people and renters are particularly likely to be overstretched financially.
- Nearly three quarters of a million over 75s have no source of income other than the State Pension and benefits. Nearly a quarter of single women aged 75 or over (400,000 women) are completely reliant on state financial support.
- Over 75s are less likely than younger pensioners to receive Pension Credit when they are eligible. Of the 1.9 million over 75s who are estimated to be eligible for Pension Credit, 39% (around 750,000 people) don’t claim.
- A third of people aged 75 and over have less than £1,500 in savings (approximately 1.6 million pensioners) and nearly one quarter have no savings at all (approximately 1.1 million pensioners).
- For older pensioners who are living below the poverty threshold, nearly half also have less than £1,500 in savings.
The report demonstrates that poverty in older age is not a thing of the past and, for older people who have little opportunity to work or increase their income in other ways, poverty can be a persistent threat.
|
Office for National Statistics (ONS) - Persistent poverty in the UK and EU: 2014
16 May 2016 |
ONS have published a report Persistent poverty in the UK and EU:2014 which shows that, while declining, older people (aged 65 and over) in the UK are more likely to experience persistent poverty than younger age groups.
Persistent poverty rates measure the percentage of the population that are at-risk-of-poverty in the current year and at least 2 out of the 3 preceding years.
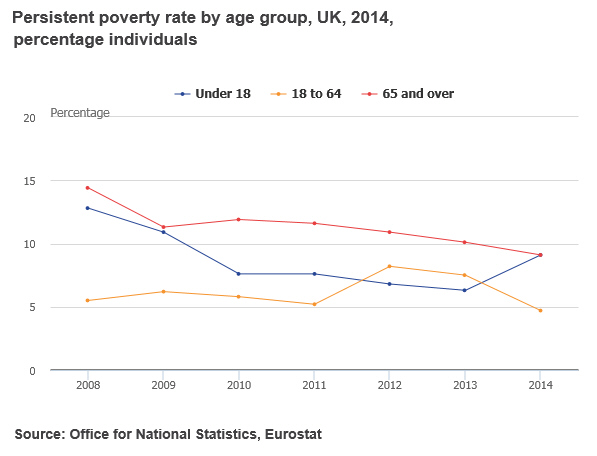
|
Royal College of Physicians - End of Life Care Audit - Dying in Hospital
30 March 2016 |
The Royal College of Physicians has published the End of Life Care Audit - Dying in Hospital, National Report for England, March 2016. Changes since 2013 include the major step, for both the NHS and the charitable sector, of the phasing out of the Liverpool Care Pathway.
Nearly half of all deaths in England occur in hospitals, 223,007 out of a total of 469,975 in 2014. In total, 142 sites from 137 out of 142 possible trusts submitted data to the organisational audit.A total of 9302 unique patient datasets (ie a complete case note review addressing each of the clinical audit questions) were submitted for the national clinical case note review sample.
Key findings included:
- Recognition of dying: Ninety-three per cent of patients whose death was predictable had documentation that they would probably die. For half the patients, recognition of dying occurred within 5 days after admission; and for half the patients this occurred less than 34 hours before death.
- Communication and treatment decisions: Where there was an advance care plan, the team took the contents into account when making decisions (91%) and it was reviewed (79%); however only 4% (415/9302) of patients had documented evidence of an advance care plan made prior to admission to hospital; A do not attempt cardiopulmonary resuscitation (DNACPR) order was in place for 94% (8711/9302) of patients’ notes at the time of death; 32% of patients had opportunities to have their concerns listened to and, of these, 94% were given the opportunity to have questions answered about their concerns.
- Communication with people important to the patient: In 38% of cases, there was documented evidence in the last episode of care that the patient’s needs had been discussed with the people important to them.
- Individual plan of care - Symptom control: Excluding sudden deaths and cases where the patient had died less than 24 hours after admission, 73% of case records showed that there had been a holistic assessment of the patient’s needs with a view to making an individual plan of care.
- Individual plan of care - Drinking and eating: In the last 24 hours of life there was documented evidence that: in two-thirds of cases the patient’s ability to drink had been assessed; thirty-nine per cent of patients were documented as drinking, and in 45% of cases that the patient had been supported to drink; In total, 18% of patients had a ‘nil by mouth’ (NBM) order in their last 24 hours. Ninety-three per cent of NBM orders had a documented reason. Twenty-three per cent of patients with an NBM order had been informed of it; 64% of the people important to the patient had been informed. The majority (54%) of the NBM decisions had involved a consultant (other than palliative medicine); 20% involved speech and language therapists (SALTs) and 16% a staff nurse.
- Individual plan of care - Spiritual care: There was documented evidence of discussion during the last episode of care regarding the patient’s spiritual/cultural/religious/practical needs with 15% of patients who were capable of participating in such discussions. In a further 27% there had been discussion with a nominated person important to the patient.It was documented that in 89% of cases, the identified spiritual/cultural/religious/practical needs had been met.
- Organisational elements - Staffing and training: In total, 13% of trusts (18/142) reported that they had specialist palliative care beds; Almost all (97%) trusts had their own specialist palliative care service; 70% also used a specialist palliative care service funded and based outside the trust.
- Organisational elements - Guidance and policies: Only 46% of trusts were involved in the Transforming End of Life Care in Acute Hospitals Programme; and only 35% of trusts are using electronic palliative care coordination systems (EPaCCSs); Ninety-eight per cent of trusts reported ‘locally developed programmes of work to support end of life care’, which probably represents the changes needed after the withdrawal of the Liverpool Care Pathway.
The report made a number of key recommendations including:
- The recognition of dying should be reviewed by a senior doctor or nurse; All professionals, especially those working with people living with chronic conditions, multiple comorbidities, and in particular people for whom future loss of mental capacity is anticipated (eg people with dementia), should initiate and encourage advance care planning;
- There needs to be better documentation of justification for NBM orders and improved communication of them to patients (if they are conscious) and to those important to them. NBM orders should only be made by a senior doctor, nurse or SALT specialist.
- Where trusts are not already using EPaCCSs or an equivalent system for record sharing, they should take steps to do so.
- All trusts should have access to specialist palliative care services 9am to 5pm, 7 days a week.
- All medical and nursing staff with responsibility for the care of dying people should attend communication skills training specifically on care in the last days/hours of life, and this should be recorded in their portfolios.
The report noted that the big opportunity for the End of Life Care Audit - Dying in Hospital (and also the biggest set of challenges) in the coming years will be to align NHS practices to the new NICE guideline (NG31).
|
Pensions Policy Insitute - The Under-pensioned 2016
01 March 2016 |
The PPI report The Under-pensioned 2016 is a report that explores differences in pension income over the last two decades and how these differences may change in the future.
The report finds positive movements in pension income for previously under-pensioned groups. Once the New State Pension has been fully phased in there will no longer be significant differences in state pension income between women, ethnic minorities, disabled people, carers, the self-employed and the average for all pensioners. However, lower private pension saving and income levels among the under-pensioned are projected to continue. These are mainly as a result of particular labour-market characteristics found more prevalently among these groups.
These pension inequalities arise from labour-market, social and regulatory issues related to inequalities experienced during working-life. Therefore, addressing ongoing differences in private pension income would involve a joint effort from government departments, employers, social services, regulatory bodies and community support groups.
|
Department for Work and Pensions - State Pension Age Review
01 March 2016 |
The Department for Work and Pensions has released a ministerial statement announcing a review of the State Pension Age.
John Cridland, recently Director-General of the Confederation of British Industry (CBI) and currently Chair of the Board of Transport for the North, has been appointed as the independent lead of the State Pension age review, which will report by May 2017.
The ministerial statement says "The purpose of the independent review is to make recommendations to the Secretary of State for Work and Pensions on factors to consider in arriving at future State Pension age arrangements. The recommendations should be affordable in the long term, fair to current and future generations of pensioners and consistent with supporting fuller working lives".
The review will not cover the existing State Pension age timetable up to April 2028 which is already legislated for.
|
ILC-UK - Tomorrow's World: The future of ageing in the UK
02 February 2016 |
ILC-UK have released a report Tomorrow's World: The future of ageing in the UK using testimony from speakers at the 2015 'Future of Ageing' conference.
The report argues that the social care system is crumbling and health care is failing to incentivise the prevention of ill health; the housing and planning system is failing to respond to ageing, resulting in people living in housing which does not meet their needs; and individuals are currently underestimating their life expectancy and risking running out of money in retirement.
ILC-UK presents a future in which health expenditure has increased debt as a proportion of GDP to 180%; more than 1 million additional care workers are required to meet the demand for social care; and millions have failed to save enough ahead of retirement.
The report suggests 10 long-term indicators of progress...
- Health must find a way to be more responsive and preventative
- Government must make progress in delivering a long term settlement to pay for social care
- Savings levels for working age adults must increase
- Average age of exit from the workforce should rise
- The number and type of homes built should be increasingly appropriate for our ageing society
- Government should make progress in facilitating greater risk sharing in accumulation and decumulation of retirement income
- We must have a more informed older consumer
- Our aspirations for retirement must be about much more than us spending more hours watching television
- Businesses should better respond to ageing
- We must strengthen the social contract between young and old
The report emphasises that without action today, the picture in 10 years time could be much worse.
|
ILC-UK - The end of formal adult social care
12 December 2015 |
ILC-UK have released a report The end of formal adult social care which they refer to as a 'provocation'.
The report says that analysis of the social care funding measures outlined in the Autumn 2015 Spending Review reveals a 'bleak future for older people needing care'.
The UK is heading towards the bottom of OECD league table for spending on care as proportion of GDP. Local authorities with the highest concentration of older people and with highest reliance on unpaid informal caring will be able to raise least from the Council Tax Precept announced in the Spending Review. This lack of investment will lead to growing reliance on informal carers with significant economic and social implications.
Key finding in the report include ...
- Approximately 1.86 million people over the age of 50 in England (1 in 10) have unmet care needs - an increase of 120,000 people (or 7%) since 2008/9.
- Data from 326 local authorities shows that the councils with the highest concentration of older people and unpaid carers will be the ones that will bring in the least amount of money from the 2% council tax precept.
- There are approximately 4.3 million people aged 50+ in England who are living alone (that's roughly 1 in 5 middle aged and older people living on their own).
The report points out that the numbers accessing care services have fallen by half a million since 2008/9 (a drop of 30%) despite a growing ageing population. The number of over 80s have risen by 800,000 in the last decade. The report also notes that there are already around 1.5 million people providing over 50 hours per week of unpaid care and that without investment the need for informal care will increase.
|
Centre for Ageing Better and ipsos MORI - Later life in 2015: An analysis of the views and experiences of people aged 50 and over
02 December 2015 |
The Centre for Ageing Better has commissioned ipsos MORI to carry out research Later life in 2015: An analysis of the views and experiences of people aged 50 and over, that investigates the factors that lead to a better later life by exploring the views of older people.
The data gathered is for England, but results are likely to be similar for the rest of the UK.
The most important factors and the things that most worry people as they age are physical health and not having enough money.
Cluster analysis of data from the English Longitudinal Study on Ageing suggests segmenting older people into six broad groups...
- Thriving boomers (21%) - typically former professionals who are financially secure and have assets in the form of property. They are generally in good health, exercise and eat well,and have good social connections with family and friends. They view themselves as fortunate with high levels of subjective wellbeing.
- Downbeat boomers (21%) - similar in terms of health and financial security to the thriving boomers, but regret life's missed opportunities and have a much lower sense of subjective wellbeing
- Can do and connected (19%) - this resilient group, despite poorer health and lower financial security, maintain high levels of happiness and subjective wellbeing as a result of high levels of social connectedness with friends and family
- Worried and disconnected (13%) - typically aged over 70 and retired, with poor social connections, not likeing to ask for support and not wanting to be a burden on others - this group has low levels of subjective wellbeing.
- Squeezed middle age (14%) - typically in their 50s with good health and still at work, this group feel financially squeezed, often 'sandwiched' with financial and/or caring responsibilities for both children and elderly parents - this group also has low levels of subjective wellbeing.
- Struggling and alone (12%) - scoring poorly on all measures, having often had health problems all their life affecting the ability to work, and with poor social connectedness, this group has the lowest levels of happiness and subjective wellbeing.
The research reinforces the importance of health, financial security and maintaining social connectedness,including through volunteering, U3A and faith groups, in maintaining happiness and subjective wellbeing in later life.
|
ILC-UK and Prudential - Understanding Retirement Journeys: Expectations vs reality
01 December 2015 |
ILC-UK and Prudential have published a report Understanding Retirement Journeys: Expectations vs reality which challenges the myth of a hedonistic retiree population.
Retirees are saving £48.7bn per year and, rather than spending on holidays and leisure, older people spend decreasing amounts on non-essentials. On average retirees think they have a 70% chance of leaving an inheritance of £50,000 or more.
From the age of 50 onwards, spending on most non-essential items begins a slow decline. With the exception of early retirement, retirement does not lead to more holidays or other leisure activities. Nor does retirement lead to an increase in eating out.
Key findings include ...
- Consumption falls during retirement: A household headed by someone aged 80 and over spends, on average, 43% less than a household headed by a 50 year old.
- Many older households continue saving throughout retirement. Individuals aged 80 and over are saving, on average, around £5,870 per year.
- Retirement does not lead to more holidays. However as we age, time at home alone increases while time spent with family and friends falls. By age 90+, watching television and spending time at home alone are the most common daily activities.
- Health appears to restrict an increasing proportion of older people from doing the things they want to do in retirement - however, the vast majority of retirees say that they are able to do the things they want
The research points to evidence of a “default retirement consumption path” where consumption falls lead to savings in later life.
|
NICE Guideline - Older people with social care needs and multiple long-term conditions
4th November 2015 |
NICE have issues a new Guideline: Older people with social care needs and multiple long-term conditions
The guideline covers planning and delivering social care and support for older people who have multiple long-term conditions. It promotes an integrated and person-centred approach to delivering effective health and social care services. The guideline is for Health and social care practitioners; Providers of care and support in health and social care services; and Older people with social care needs and multiple long-term conditions (including both physical and mental health conditions), and their carers.
The guideline includes recommendations on ...
- Identifying and assessing social care needs
- Care planning
- Supporting carers
- Integrating health and social care planning
- Delivering care
- Preventing social isolation
- Training health and social care practitioners
|
Joseph Rowntree Foundation - The costs and benefits of paying all the lowest-paid care home workers in the UK the Living Wage
26th October 2015 |
The Joseph Rowntree Foundation has published new research: The costs and benefits of paying all the lowest-paid care home workers in the UK the Living Wage.
This research investigates earnings below the Living Wage for staff in care homes for older people, what the costs and benefits might be of paying all staff the 'living wage', and how this pay increase could be funded.
- The estimated annual wage cost of paying the Living Wage to all care home staff in 2014 is £830 million for the UK, increasing to almost £1 billion when National Insurance and pension contributions are factored in
- Paying higher wages reduces the need for in-work benefits, conservatively estimated at £19 per week per household in 2014
- The new National Living Wage announced in the Summer 2015 budget will affect at least 50% of care home workers. Including National Insurance and pension contributions, it would cost £387 million per year.
- Care homes with self-funded residents are most likely to be able to afford a wage increase. Providers heavily dependent on local authority funding are least likely, given that local authorities fees are currently failing to cover the cost of residential care.
- The most compelling funding option is for central government to make more funds available to care home providers, given that it will receive additional funds from increases in tax and national insurance receipts and reductions to in-work benefits payments. The net public sector cost of the Living Wage would be £286 million per year.
|
Age UK - Briefing: The Health and Care of Older People in England 2015
21st October 2015 |
Age UK have published a briefing: The Health and Care of Older People in England 2015 which provides a useful overview of many aspects of the current health and care of older people in England.
In summary, the briefing concludes that all the figures point in the same direction -
"The numbers of older people in England are steadily growing, and the proportion with long term conditions is growing faster still, but investment in health care overall is failing to keep pace with the impact of demographic change and other factors driving higher demand, and spending on social care has fallen quite spectacularly over the last five years."
On the whole it is the primary and community based services on which many older people depend in order to sustain their independence which have seen the sharpest falls or where supply is most obviously failing to meet rising demand.
The briefing contains over 40 charts and graphs providing detailed information, but the key points are ...
- The population is ageing and older age groups are more likely to have health conditions, many of which are preventable and most of which are manageable
- There has been a reduction in funding and it is targeted at fewer people - those with the highest need
- Unmet need is rising - in 2015 more than a million older people in England have at least one unmet need for social care compared with 800,000 in 2010.
- Funding increases have not kept pace with rising demands and costs
- There are disparities in funding between different types of health service with in 2012/13 (at 2014/15 prices) £46 billion spent on hospital care compared with £10 billion on community health services, £9 billion on mental health services and £8 billion on GP services. Increases in staffing have gone mainly to hospitals.
- There are growing demands on both hospital and GP services with stress on the system including concerns about quality and increased waits for appropriate care outside of hospital
|
ONS - Insights into Loneliness, Older People and Well-being, 2015
1st October 2015 |
ONS have published a report Insights into Loneliness, Older People and Well-being that focuses on older people's well-being, loneliness and some of the risk factors associated with loneliness such as living alone, housing tenure, marital status, ill health and support networks.
The report uses data from the personal well-being dataset and the Opinions and Lifestyle Survey for the financial year ending 2015.
The data reveals that people aged 65 and over tend to have lower levels of anxiety and higher levels of happiness, life satisfaction and a feeling that activity is worthwhile than people of 'working age', although this tends to drop away again after age 80.
One possible reason for the drop in wellbeing after age 80 may be an increase in levels of loneliness with 1 in 3 (33%) of people aged 80 and over reporting feeling lonely.
The report details the risk factors associated with loneliness in older age
- living alone
- renting
- being widowed
- being in bad or very bad health
Older people who report bad or very bad health are 2.5 time more likely to report being lonely than those in good health.
|
Government Office for Science - Foresight: 'Future of an ageing population'
September 2015 |
Between June and September 2015, the Government Office for Science has published 22 evidence reviews that it has commissioned as part of the Foresight 'Future of an Ageing Population' project. The reviews analyse the opportunities and challenges of an ageing society.
The reviews cover a wide range of topics about ageing, including retirement income, life expectancy and inequalities, health and social care, prevention and wellbeing, and life-long learning and employment.
The reports can be downloaded from the Foresight - Future of an Ageing population website ...
|
NICE Guideline - Home care: delivering personal care and practical support to older people living in their own homes
23 September 2015 |
NICE have issues a new Guideline: Home care: delivering personal care and practical support to older people living in their own homes
The guideline covers the planning and delivery of person-centred care for older people living in their own homes. It aims to promote older people's independence and to ensure safe and consistently high quality home care services.
The guideline includes recommendations on ...
- Ensuring care is person centred
- Providing information about care and support options
- Planning and reviewing home care and support
- Delivering home care, including recommendations on the length home care visits
- Joint working between health and social care
- Ensuring safety and safeguarding people using home care services
- Recruiting, training and supporting home care workers
|
In Control, Lancaster University and Think Local Act Personal - Personal health budget holders and family carers - (POET 2015)
10 September 2015 |
In Control, Lancaster University and Think Local Act Personal have published the findings of the third personal outcomes evaluation tool (POET) survey of personal health budget holders and their carers.
Over 300 personal health budget holders from 31 different areas across the country and 247 carers from 37 different areas completed the survey.
The most common way to use their budget was on care and support services (59.6%), followed by personal assistants (48.3%), community and leisure services (26.8%) and equipment (25.2%).
Over 80% of personal health budget holders reported their budget having a positive impact on their quality of life, independence and arranging support.
Over 60% reported their budget having a positive impact on their relationships with people paid to support them, as well as a positive impact on their friendships, physical and mental health.
Over three quarters of carers said that having a personal health budget had improved day to day stress, quality of life of the carer, quality of life of the person, choice and control the carer has in life.
|
Ready for Ageing Alliance - The myth of the baby boomer
18 August 2015 |
The Ready for Ageing Alliance has published a brief report The myth of the baby boomer rebutting the notion that the so-called 'baby boomers' are a homogeneous generation of older people who are benefitting at the expense of younger generations.
The report rebuts the 'lump of labour' fallacy that older people in work are taking the jobs of younger people, reminding the reader that the same arguments were used to discourage women from working.
The report also challenges notions that the current generation of older people are all fit and healthy and can look forward to security in retirement with generous pension provision
The report includes evidence that...
- Whilst many boomers have benefitted from house price inflation, just under half of those aged 55-64 in England fully own their property and 24% are still renting.
- Whilst some boomers can expect to live a long time in good health, men in the most deprived parts of the England can expect to live to 52.2 year in good health compared with 70.5 in the least deprived areas. 6.7 million people aged 45-64 have a long standing illness or a disability.
- Whilst some boomers benefitted from free education, under one in five of those aged 55-64 in the UK have a degree.
- Whilst some boomers will retire with good pension provision, almost three in ten of 55-64 year olds in Great Britain do not have any pension savings (nearly 2 million people).
The implications of the report are that, although it may be possible to demonstrate that, in some respects, the current generation of older people are in a better situation than future generations can look forward to, this is not the fault of the current older generation who grew up in an expectation that life would always improve for each future generation. These chance benefits should not be used as an issue to divide generations but as a spur to greater efforts to create improvements for future generations.
|
Nesta - The NHS in 2030: a people-powered and knowledge-powered health system
21 July 2015 |
Nesta has published The NHS in 2030, an optimistic view of what a health system would look like in 2030 if new knowledge is used differently and more people play a role in managing health.
The four axes of change set out in the report are: the promise of precision medicine; a health knowledge commons stretching beyond traditional actors; a system powered by more people and new kinds of relationships; and taking advantage of contemporary behavioural insights.
The report concludes that achieving a successful health system powered by people and knowledge in 2030 will require new policy and support mechanisms including...
- Digital platforms and widely agreed protocols for developing new kinds of health knowledge and responding to the latent demand for taking part in healthcare.
- Prototypes for health data sharing that concentrate on understanding emerging attitudes to digital privacy.
- An institution that supports and evaluates for People Powered Health research.
- A central institution to set standards and mandate processes that will maximise the clinical and research value of large genomic and other data sets as they become available.
|
Carers UK - State of Caring 2015
20 May 2015 |
Carers UK carries out an annual survey of carers to build a picture of the state of caring in the UK.
The State of Caring 2015 report, based on the experiences of 4,500 carers, reveals the effects of recent service reductions and the impact of caring on mental health, social life and personal finances.
Key findings include ...
- Over half (55%) of carers say that they are worried about the impact of cuts to care and support services over the next year.
Over half (53%) of carers responding to the survey have experience of social care services such as home care or respite care. Of these, 27% report positive experiences of these services (7% excellent and 20% good) while 21% report negative experiences (8% bad and 13% terrible). Half say that their experiences have been mixed (42%) or fair (10%). One third (33%) of carers with experience of social care services say that they have refused or stopped using a service altogether because of concerns over quality.
- 82% of carers report that caring has had a negative impact on their health, 2% more than in 2014. Three quarters (74%) of carers find it difficult to get a good night's sleep (5% more than last year) while nearly half (47%) struggle to maintain a balanced diet. Four in ten (41%) have experienced an injury or their physical health has suffered as a result of caring.
This has consequences for carers' mental health, with 84% saying they feel more stressed, 78% saying they feel more anxious, and 55% reporting that they have suffered from depression as a result of their caring role - significantly more than in 2014. Over three quarters (76%) of carers responding to the survey were concerned about the impact of caring on their health over the next year.
- Previous Carers UK's research has found that many carers experience social isolation and loneliness as a result of caring. This is reflected in the State of Caring Survey 2015, with well over half (62%) of those carers who are struggling to make ends meet saying they are cutting back on seeing friends or family to save money.
- Nearly half (48%) of carers who responded to the survey were struggling to make ends meet. Of those struggling to make ends meet, 41% are cutting back on essentials like food and heating, 26% are borrowing from family and friends and 38% are using up their savings to get by - suggesting that the squeeze on carers' finances is not sustainable in the long term.
- Of carers responding to the survey, 45% say that financial worries are affecting their health. Over half (52%) are worried about the impact of cuts to social security over the next year and a similar number (54%) are worried about their finances.
- Over three million carers in the UK combine work with their caring responsibilities, including over two million who are working full-time.
Of full-time or part-time employees responding to the survey, over two thirds (68%) have used their annual leave to care and 46% have done overtime to make up hours spent caring.
Half (51%) of carers responding to the survey have given up work to care and 12% have retired early to care. A fifth (21%) reduced their working hours while 13% have had to take a less qualified job or turned down promotion to fit around caring.
Of those who gave up work, retired early or reduced working hours, 65% said the stress of juggling work and care was a contributing factor, 30% said it was because there are no suitable care services and 22% said care services are too expensive. 15% said that the leave available from work was insufficient to be able to manage caring alongside work and 18% were unable to negotiate suitable working hours.
Six in ten (60%) working carers are worried about their ability to remain in work over the next year.
|
Care Act 2014: statutory guidance for implementation
23 October 2014 |
The Department of Health has issued Statutory guidance to support implementation of part 1 of the Care Act 2014 by local authorities.
The Care and Support Statutory Guidance associated with the Care Act sets out how the Act will work in practice when the first phase of the reforms comes into effect in April 2015. There is also an easy to read summary.
The guidance covers...
- General responsibilities and universal services including...
- Promoting wellbeing
- Preventing, reducing or delaying needs
- Information and advice
- First contact and identifying needs
- Charging and financial assessment
- Person-centred care and support planning
- Adult safeguarding
- Integration and partnership working
- Moving between areas: inter-local authority and cross-border issues
The Local Government Association (LGA) has produced a useful 'on the day' summary briefing
|
Ready for Ageing Alliance - Manifesto
15 September 2014 |
The Ready for Ageing Alliance has published its manifesto setting out ideas for how policymakers can better respond to the challenges of ageing.
The Alliance believes that the growing numbers of people in later life are a cause for real celebration but that we need to do a lot more to respond to both the challenges and the opportunities that longevity brings
The manifesto sets out detailed recommendations for public policy covering housing; health and social care; the economy and communities and calls for Government to take the lead, with a single point of contact, at Cabinet level, responsible for age and ageing policy.
The manifesto declares that we should...
- Stop seeing ageing as being just about older people - if we wait until we are 60 or 70 to prepare we'll have left it too late.
- End age discrimination - Legislation has gone some way to preventing discrimination on grounds of age but bizarrely financial services are exempt and hidden discrimination remains in many walks of life
- Stop operating hospitals on a model designed for the past - Staff/patient ratios on hospital wards for older patients are often lower than on general wards, yet older people often need more help - e.g. to eat and drink
- Stop undervaluing the over 65s, who currently spend a massive £2.2 billion a week and contribute £61billion to the economy through employment, caring and volunteering.
- Stop ignoring the fact that many older workers are forced to leave the labour market early. Start building more flexible work opportunities to make it possible for family members of all ages juggle work and care for older relatives
|
Alzheimer's Society - Dementia UK: second edition
10 September 2014 |
The Alzheimer's Society society has published a second edition of its key publication Dementia UK. This edition includes updates of the authoritative UK dementia prevalence rates published in the 2007 first edition.
Although the overall prevalence of dementia for the over 65s remains at 7.1%, the number of identified cases of early-onset dementia, has risen from 15,000 in the 2007 report to 40,000 in the current report. It is likely that this results from increased rates of diagnosis and population increase rather than a real change in prevalence.
Key findings include...
- At the current estimated rate of prevalence, there will be 850,000 people with dementia in the UK in 2015
- The number of people with dementia in the UK is forecast to increase to over 1 million by 2025 and over 2 million by 2051.
- There are over 40,000 people with early-onset dementia (before the age of 65 years) in the UK
- The total cost of dementia in the UK is £26.3 billion
- Two thirds of the cost of dementia (£17.4 billion) is paid by people with dementia and their families, either in unpaid care (11.6 billion) or in paying for private social care.
|
The King's Fund - final report from the independent Commission on the Future of Health and Social Care in England.
5th September 2014
|
The King's Fund has launched the final report from the independent Commission on the Future of Health and Social Care in England.
The commission, headed by Dame Kate Barker CBE, proposes a new approach that redesigns care around individual needs regardless of diagnosis, with a graduated increase in support as needs rise, particularly towards the end of life.
Key recommendations of the commission include...
- moving to a single, ring-fenced budget for the NHS and social care, with a single commissioner for local services.
- a new care and support allowance, would offer choice and control to people with low to moderate needs while at the highest levels of need the conflict between who pays for care, the NHS or the local authority, will be removed
- individuals and their carers should benefit from a much simpler path through the whole system of health and social care that is designed to reflect changing levels of need.
- a focus on more equal support for equal need, which in the long term means making much more social care free at the point of use.
- new NHS charges and private insurance options are , in general, rejected in favour of public funding
- the commissions makes proposals for a single, ring-fenced budget and single local commissioner
- the commission proposes funding changes, including changes to National Insurance contributions, to meet the additional £5 billion that would be required to improve social care entitlements.
- the commission proposes a comprehensive review of various forms of wealth taxation needs to be undertaken with a view to generating additional resources that will be needed for health and social care in future years.
In parallel, the Kings Fund have also published an illustrated summary and a written overview of the final report.
|
Department for Work and Pensions - Fuller Working Lives - A Framework for Action.
9th June 2014
|
The UK Government, Department for Work and Pensions has published Fuller Working Lives - A Framework for Action.
The framework document makes the case for older people to lead fuller working lives. It outlines how early exit from the labour market can have serious implications for the health, wellbeing and incomes of individuals and comes at a significant cost to the economy, business and society as a whole.
- Leaving work before State Pension age makes it much more difficult to maintain living standards into retirement.
- Early labour market exit damages public finances and the wider economy
- Early labour market exit can be damaging for business
According to the framework, the interplay of factors that lead people to feeling forced to stop work vary from person to person. However, it is known that the major factors that influence decisions to leave work are
Health conditions; Disability; Caring responsibilities; Redundancy; Workplace factors and Financial security.
As background information to the support the framework document, DWP have also published background evidence, charts and tables and an infographic. Key findings are...
- there are more over 50s in employment than ever before and the employment rate of older people is still rising
- early labour market exit is still a problem, with around 2.9 million people currently out of work aged between 50 and State Pension age
- over half of men and women have already stopped working before they reach State Pension age
- 1 in 6 men and 1 in 4 women who had recently reached State Pension age hadn’t worked since at least age 55
|
The Care Act 2014
14 May 2014
|
On 14th May 2014 the Care Bill received royal assent and became The Care Act 2014.
The Act includes:
- a new framework of duties on local authorities in relation to the provision of social care, including assessment of care needs, duties to arrange care, funding and the Dilnot care cap. The provisions include:
- new requirements to assess and meet the needs of carers
- new provision for a single national test of eligibility for local authority involvement in arranging and funding care
- provisions to increase transparency about costs of care and change the balance between self-funded care and local authority funded care
- a cap on total care expenditure of £72,000 but excluding residential care 'hotel' fees of approximately £12,000 per annum
- a universal deferred payments scheme where non housing assets held are less than £23,250, allowing the deferral of the payment of residential care fees, up to 70-80% of the value of the main residence ,secured on the main residence and subject to an administration fee and interest charged at 3½ - 5%.
- a requirement to arrange for the provision of prevention services
- a duty to promote the wellbeing of individuals and promote integration between health and social care services
- powers for local authorities to delegate many of their social care functions
- duties on local authorities with respect to safeguarding of adults receiving social care
- provisions with respect to the regulation of care providers, including:
- a duty of candour, applying to all health and social care providers regulated by the CQC
- a new criminal offence for some care providers of giving false or misleading information
- changes to the CQC regulatory regime, including new powers to monitor the financial sustainability of providers
- provision for the Human Rights Act to apply to some private sector care providers
- a statutory basis for the Better Care Fund, i.e. powers to direct Clinical Commissioning Groups to use NHS funding in projects for developing integrated health and social care services
- new arrangements in respect of discharge from hospital and after-care under section 117 of the Mental Health Act
The government created a number of factsheets to accompany the bill.
|
The Pensions Act 2014
14 May 2014 |
On 14th May 2014 the Pensions Bill (2013-14)received royal assent and became The Pensions Act 2014.
The main provisions of the Act are...
- State pension reform (the single-tier pension)
The single-tier pension will replace the basic state pension and additional state pension with a flat-rate pension that is set above the basic level of means-tested support for people who reach state pension age on or after 6 April 2016.
In steady state, 35 qualifying years of National Insurance contributions or credits will be needed for individuals to receive the full amount. Those with fewer than 35 qualifying years will receive a pro-rated amount. Entitlement to the pro-rated amount will be subject to the individual having a minimum number of qualifying years, which will be no more than 10 years.
- Voluntary national insurance contributions (Class 3A) - State Pension top-up
The Act provides for a new type of voluntary national insurance contribution, called Class 3A. This will allow pensioners who reach state pension age before 6 April 2016 to top-up their additional state pension.
The rates are the same for males and females. The contribution required for an extra £1 pension per week for a person aged 65 is £890. For £4,450, the individual could receive an additional £260 per year for life, increased in line with prices and inheritable on death in the same way as existing additional State Pension: with a minimum of 50% for the surviving spouse or civil partner. For a 70 year old the rate reduces to £779 and at age 75 the rate is £674.
- Bringing forward the increase in the State Pension age to 67
This change will mean that the state pension age will gradually rise from 66 to 67 between 2026 and 2028.
- A framework for future changes to state pension age
The framework provides for a regular review of the state pension age, based around the principle that people should spend a given proportion of their lives receiving a state pension.
- Bereavement benefits
The Act contains provisions to introduce Bereavement Support Payment to replace the existing bereavement benefits for new customers. The intention is to simplify the system by moving to a more uniform payment structure with support focused on the period immediately following bereavement and a single contribution condition.
- Automatic transfers
The Act introduces a framework to provide for a system of automatic transfers of small pension pots so that a person's pension will follow them to their new pension scheme when they change jobs. This will help people to keep their pension savings in one place.
- Automatic enrolment
The Act contains some clarifications relating to automatic enrolment. Under automatic enrolment, employers and their employees, who are at least 22 and under State Pension age and earn more than £10,000 a year, make regular contributions to a workplace pension scheme, unless they choose actively to opt out. The government also contributes through a tax-break.
- Charges and quality standards in workplace pensions
The Act contains powers to allow the government to introduce minimum governance and administration standards and restrict charges in workplace pensions. The government announced that it will use these powers to restrict high and unfair charges and strengthen governance in defined contribution workplace schemes.
DWP have also published an Impact Assessment.
|
Commission on the Voluntary Sector & Ageing - Age of opportunity
1 April 2014
|
NPC, working in partnership with ILC-UK, have published a report Age of opportunity: Putting the ageing society of tomorrow on the agenda of the voluntary sector today to mark the launch of the Commission on the Voluntary Sector & Ageing.
The report provides context on the voluntary sector and the country’s ageing population, and then covers a number of areas thought to be of particular interest: relations between the different sectors, health and well-being, technology, volunteering and trusteeship, employment and fundraising.
The report asks a series of questions: in the context of an ageing society including: what will the voluntary sector look like in 20 years’ time? How will change impact the beneficiaries the voluntary sector works with? What will it mean for the workforce, and volunteering and fundraising strategies? And how will these changes affect the voluntary sector itself?
|
The King's Fund - Making our health and care systems fit for an ageing population
6 March 2014
|
The King's Fund has launched the report Making our health and care systems fit for an ageing population.
The report's view is that improving services for older people requires the consideration of each component of care, since many older people use multiple services, and the quality, capacity and responsiveness of any one component will affect others.
The key components considered are:
- healthy, active ageing and supporting independence
- living well with simple or stable long-term conditions
- living well with complex co-morbidities, dementia and frailty
- rapid support close to home in times of crisis
- good acute hospital care when needed
- good discharge planning and post-discharge support
- good rehabilitation and re-ablement after acute illness or injury
- high-quality nursing and residential care for those who need it
- choice, control and support towards the end of life
- integration to provide person-centred co-ordinated care.
|
Department of Health - Open consultation on 'Fundamental standards for health and social care providers'
23 January 2014
|
The Department of Health has launched an open consultation on Introducing Fundamental Standards, a consultation on proposals to change CQC registration regulations.
DH say that the proposals to amend the CQC registration requirements are part of a wide-ranging set of changes designed to improve the regulation of health and social care providers, and provide assurance that service users receive safe, quality care and treatment.
The purpose of the changes is to introduce fundamental standards; to make regulations more effective and improve enforcement against them; to be outcome focused; and to reduce the burden on business.
Easy read versions , draft regulations and an impact assessment are available from the .gov.uk website.
The consultation ends on 4th April 2014.
|
ONS - What does the 2011 Census tell us about the "oldest old" living in England & Wales?
09 December 2013 |
The Office for National Statistics has published its latest analysis about the older population of England and Wales, drawn from the 2011 census, What does the 2011 Census tell us about the "oldest old" living in England & Wales?.
Key facts about the "oldest old" (those aged 85 and over) include...
- On Census Day 2011 there were 1.25 million people aged 85 or over who were usually resident in England & Wales. This compared to 1.01 million in 2001.
- In 2011, women outnumbered men in this age group by 2:1, but there was a larger percentage increase in the number of men (45%) than women (16%) over the decade.
- In 2011, about one in ten men and one in five women aged 85 and over lived in a communal establishment, with the remainder living in a private household.
- For every 100 women aged 85 or over, 77 were widowed, 13 were married and 10 were either single, separated or divorced. Out of every 100 men aged 85 and over, 43 were widowed, 48 were married and nine were either single, separated or divorced.
- 31% of men and 25% of women aged 85 and over in 2011 considered that they had very good or good general health. This compared to 24% of men and 26% of women who reported that they had bad or very bad health.
- A larger proportion of those aged 85 and over were providing unpaid care in 2011 than in 2001; 8.8% in 2011 compared to 5.0% in 2001. Over half of those aged 85 and over who provided care in 2011 were providing 50 or more hours of care in an average week.
|
Government response to the Justice Committee’s report on Older Prisoners
November 2013 |
The Ministry of Justice has published the Government response to the Justice Committee’s Fifth Report of Session 2013-14: Older prisoners. The committee report made 30 recommendations. The Government response accepted that the treatment of older offenders should not be based on strict chronological age but individual need, informed by age and disability.
They accept that a formal analysis of the prison estate, by the National Offender Management Service (NOMS), is required to determine the extent to which older prisoners needs are being met by prison buildings and how this could be improved..
It is agreed that improved screening is required to ensure older offenders are appropriately allocated to establishments with the necessary facilities and that appropriate activies are available for those prisoners unable to participate in the 'normal' regime.
The responses included comments on health, mental health and social care needs and accepted the need to focus on the changing profile of the prison population, and to ensure that there is adequate provision to meet needs, especially prisoners’ needs for social care.
|
Department of Health - "Integration pioneers leading the way for health and care reform"
01 November 2013 |
The Department of Health (England) has identified 14 areas leading the way for health and care reform by bringing services closer together than ever before. The achievements in the announcement by Care and Support Minister Norman Lamb included
- 2,000 fewer patient admissions over a two and a half year period, achieved through teams of nurses, social workers, occupational therapists and physiotherapists working together to prevent crises
- Reducing waiting times from eight weeks to 48 hours at physiotherapy services by making professionals work closer together
- Setting up a crisis house where people who suffer mental health problems can get intensive support
The fourteen areas were Barnsley, Cheshire, Cornwall and Isles of Scilly, Greenwich, Islington, Leeds, Kent, North West London, North Staffordshire, South Devon and Torbay, Southend, South Tyneside, Waltham Forest and East London and City, and Worcestershire.
|
The Economic Contribution of Older Londoners
17 October 2013
|
GLA Economcs and the Mayor of London have launched a report The Economic Contribution of Older Londoners estimating the economic contribution of Londoners age 50 and over from employment, caring and volunteering.
The report values older peoples economic contribution from volunteering at at £980 per older volunteer per year, from childcare by grandparents at between £3,200 and £6,300 per year for each grandparent providing childcare, for care for other adults at £14,600 per year for each giver of care and £57,000 per year for each older person in employment.
The report estimates the total economic contribution of older Londoners at £53.1 billion, mainly from paid employment but with £4.7 billion from the care of other adults.
|
Healthwatch England first Annual Report
8 October 2013
|
Healthwatch England has presented its first annual report to parliament.
The report provides an overview of the current state of health and social care in England including a survey and the results of a face to face deliberative event to determine what people really think about the care they receive.
It includes an explanation of the role of Healthwatch England and local Healthwatch and a report of its activities.
The survey found that, although 72% of the public say they get good quality care, 1 in 3 people say they are worried about basic levels of safety, with someone they know having experienced a serious mistake, abuse or preventable illness or death.
|
Equality and Human Rights Commission - Close to Home
8 October 2013
|
The Equality and Human Rights Commission has published Close to Home, a report outlining the experience of older people receiving care at home, the effects of different commissioning practices for home care serices, other challenges to older people's human rights and how threats to human rights in home care can be brought to light.
The report recommends that
- the gaps in the current legal system are closed so that older people receive better protection
- local authorities need to do more to incorporate human rights into the way they commission care services and overcome barriers to making complaints
- older people and their families need to have better access to information when making choices about care provision
- clearer guidance on human rights obligations should be provided to local authorities.
Summary and easy read versions are available from the .
|
ONS - What does the 2011 Census tell us about Older People?
6 September 2013
|
The Office for National Statistics has released results about older people from the 2011 census for England and Wales. The report,What does the 2011 Census tell us about Older People? reveals a number of key points:
- In 2011, 9.2 million (16 per cent) of usual residents of England and Wales were aged 65 and over, an increase of almost one million from 2001.
- Fifty Seven per cent (5.3 million) of those aged 65 and over in 2011 were married or in a civil partnership but the proportion of those aged 65 and over who were divorced almost doubled from 5.2 per cent in 2001 to 8.7 per cent in 2011
- Just under a third (31 per cent) of those aged 65 and over were living alone in 2011; this was a decrease from 34 per cent in 2001.
- Ten per cent of people aged 65 and over were economically active, Ninety per cent were economically inactive including 86% retired but the proportion of the population aged 65-74 who were economically active in 2011 (16 per cent) was almost double the proportion in 2001
- Half (50 per cent) of all usual residents in England and Wales aged 65 and over living in households reported very good or good health in 2011 compared with 88 per cent for those aged under 65
- Fourteen per cent of older people living in households in England and Wales provided unpaid care in 2011, compared to 12 per cent in 2001. The largest increase in proportion was for those aged 65 and over providing 50 hours or more unpaid care a week: up from 4.3 per cent (341,000) in 2001 to 5.6 per cent (497,000) in 2011
|
Department of Health to fund housing to help older and disabled people to live independently
24 July 2013 |
The Department of Health (England) has released funding for building projects producing homes that will support older and disabled people to live independently.
In 2012 the government asked local authorities to bid for a share of £300 million to boost the supported housing market. The Department of Health has now allocated funding to build 3,544 new homes.
Affordable supportive housing is designed to be accessible and aid independent living by having, for example:
- very few or no stairs
- cupboards that are at a reachable height for wheelchair users
- adapted bathrooms that are easy to access for older or disabled people
- handrails to reduce the chance of falls
|
Demos - Commission on Residential Care (CORC)
23 July 2013
|
Demos is hosting a Commission into the future of residential care chaired by former Care Services Minister Paul Burstow MP.
The Commission will consider the financial, operational, governance and cultural aspects of residential care and how these might be improved.
The Commissioners will gather evidence from charities, care providers, current care home residents and staff and members of the wider public, particularly the ‘next generation’ of care home users to assess future demand. They will also gather evidence from the public and organisations working in the care sector and make site visits, carry out interviews with practitioners and focus groups and with current and future care users as well as exploring best practice examples from abroad.
The commission will report in summer 2014.
|
Government reponse to the House of Lords Select Committee on Public Service and Demographic Change - Ready for Ageing?
18 July 2013
|
The Government has published a reponse to the, 13th March, House of Lords Select Committee on Public Service and Demographic Change - Ready for Ageing? report.
The response outlines the programme of reforms that the government has already put in place and lists additional activity since the House of Lords report was published including backing for the Big Lottery Fund 'Centre for Ageing Better', 'Living Well for longer' a call to reduce avoidable premature mortality, the May 2013 Pensions Bill to introduce a single tier flate rate state pension and a commitment to pooled health and social care budgets.
The Government will ask the Government Chief Scientist to lead an analysis of the challenges of an ageing society; publish an action plan to extend working lives and develop the detail of an NHS England plan for vulnerable older people in primary care and urgent and emergency care.
Lord Filkin, chair of the House of Lords committee has called the response "weak and failing to give leadership on the biggest social change facing our society."
|
House of Commons Justice Committee’s Fifth Report of Session 2013-14 - Older Prisoners
13 July 2013
|
The House of Commons Justice Committee has published its Fifth Report of Session 2013-14 on Older Prisoners.
The report looks at the characteristics of older prisoners, the suitability of the prison estate and regimes, the health and social care of older prisoners, resettlement, and the possibilities of a national strategy for older prisoners.
The committee's notes that the duty to treat each prisoner as an individual should not inhibit the identification of common features among the older prisoner population that can inform policy.
Its recommendations include that the National Offender Management Service (NOMS) should conduct a comprehensive analysis of prisons’ physical compliance with disability discrimination and age equality laws and that, in general, older prisoners should not be segregated.
There should be better coordination between healthcare and prison services, better training and awareness of mental health problems, improved provision of social care and that that NOMS should prepare guidance for prisons in liaising with local authorities social care teams,
Work into developing new guidelines in the use of restraint in clinical environments provides an opportunity to assess whether the balance between security and compassion is sufficiently achieved..
The committee conclude that the growth of the older prison population and the severity of the needs of that population, warrant a national strategy in order to provide for them effectively.
|
2013 Spending Review
26 June 2013 |
On 26th June 2013, George Osborne, Chancellor of the Exchequer, announced the government's spending plans for 2015, after the next general election.
A number of announcements made will have a direct impact on older people
- There will be moves to integrate health and social care with, from 2015, a £3.8bn health and social care budget for jointly commissioned programmes.
- From 2015 there will be an overall 'system wide' cap on welfare and benefit spending. This will include pensioner benefits but not the state pension.
- The winter fuel allowance will be subject to a temperature test so that pensioners living abroad in hot countries will no longer be eligible.
The review takes place against the background of earlier announcements which will impact on older people including local authority budget cuts of 10% on social care services and a question over whether the announced, and widely supported, investment in better integrated care will result in the hoped for new frontline services for older, disabled people, the seriously ill and their carers.
Details of the spending review are available from HM Treasury.
|
Kings Fund - Commission on the Future of Health and Social Care in England
26 June 2013
|
The King's Fund has launched a Commission on the Future of Health and Social Care in England.
The Commission will go back to first principles, fundamentally re-examining the post-war settlement,asking if it remains fit for purpose and, if so, how the NHS and social care systems could be brought closer together.
Chaired by Kate Barker, there will be four commissioners: Geoff Alltimes; Lord Bichard; Baroness Greengross and Julian Le Grand.
The Commission will produce an interim report in early 2014 and a final report by September 2014.
|
Kings Fund - Paying for Social Care: Beyond Dilnot
21 May 2013
|
The King's Fund has published Paying for Social Care: Beyond Dilnot providing a history of recent social care reform and detailing present and future 'pressures'. The report provides a summary of the Dilnot proposals and ways forward for the funding of health and social care.
The report suggests four key priorities to provide a 'roadmap' for social care reform
- prepare detailed planning arrangements for implementing the Dilnot proposals
- a single strategic budget settlement for the NHS and Social Care
- Health and welfare boards to play a key leadership role in the transformation of local health and care services
- a fundamental review of the way in which health and social care entitlements,benefits and funding are organised
|
Care Quality Commission - 'Time to Listen' - two reports on the dignity and nutrition inspection programme
19 March 2013 |
The Care Quality Commission has published 'Time to Listen', two reports on an inspection programme that looked at the care provided to older people in Care Homes and NHS Hospitals.
The programme focused on whether older people are treated with respect and dignity and get the food and drink that meets their needs.
In Care Homes: homes meeting CQC standards tended to promote a culture of care that put residents first, clearly understanding the preferences and care needs of residents. Homes that kept an accurate record of residents care, needs and prevences were more likely to reach the relevant standards. In successful homes, staff saw residents as individuals. CQC inspectors identified that problems commonly arise from cultures of care that put tasks before people.
In NHS Hospitals: an inspection of 50 hospitals revealed that while the proporton of hospitals where patients were given a choice of foods to meet their nutritional needs and were helped to eat and drink when necessary has imoroved since 2011 (83% --> 88%), the proportion always treating patients with dignity and respect has declined (88% --> 82%).
As with care homes, hospitals that performed best had good record keeping and systems 'firmly' in place to record and monitor patients' needs.
|
House of Lords Select Committee on Public Service and Demographic Change - Ready for Ageing?
13 March 2013
|
The House of Lords Select Committee on Public Service and Demographic Change - Ready for Ageing? report gathered evidence on how well the UK goverment and public services are prepared to adapt to the needs of an ageing population.
While welcoming increased longevity that would see, for example, the number of people in England aged 85 and over more than double between 2010 and 2030, the committee recognised a number of challenges and reached a number of key conclusions and recommendations including
- Government and employers need to work to end 'cliff-edge' retirement allowing for greater flexibility in transition
- Government and the pensions industry need to tackle the uncertainty of 'defined contribution' pension schemes
- The financial services industry should improve the quality of, and hence confidence in, equity release schemes
- Radical change is needed in the way health and social care service are provided with services working well 24 hours per day, 7 days per week. The structural budgetary split between health and social care is no longer sustainable.
- Government should set out a framework for transforming healthcare before the 2015 election and political parties should prepare position papers.
- There is a need to plan an adequate supply of appropriate market and social housing for both younger and older people.
- The government should set out the issues and challenges of an ageing society, together with their vision for public service provision, in a White Paper to be published well before the next general election
- The government elected in 2015 should quickly set up two commissions to report on
- financial service provision - including pensions, savings and equity release
- the structure and funding of health and social care to meet the needs of an ageing population
The report and evidence presented are both available from the select committee website.
|
Care Quality Commission - Care Update
12 March 2013 |
The Care Quality Commission Care Update report gives CQC’s latest view of the performance of care services in England in the nine-month period up to 31 December 2012
This Care Update finds that the health and social care system is struggling to care adequately for people with dementia. This is having an impact on hospital capacity and resources. In more than half of PCT areas in the country, people with dementia living in a care home are more likely to go into hospital with avoidable conditions (such as urinary infections, dehydration and pressure sores) than similar people without dementia. Once in hospital, people with dementia are more likely to stay there longer, to be readmitted, and to die there.
The report indicates that these findings highlight a system-wide challenge of integrating care across hospitals and care homes, and also raise questions about whether the right services for people with dementia are being commissioned and whether NHS services can cope.
|
Alzheimer's Society report - 'Low expectations: Attitudes on choice, care and community for people with dementia in care homes'
26 February 2013 |
The Alzheimer's Society report Low expectations suggests that 80% or more of residents in care homes have dementia or significant memory problems. this is much higher than the prevalence found in CPA's own analysis of Bupa care home resident census data which set the level at about 50% but with regional variations and variations with age. The CPA analysis found, surprisingly, that, unlike in the community, the prevalence of dementia in care home does not increase consistently with the age of the resident. The oldest care home residents are often admitted because of frailty and an inability to cope at home, but without a specific health condition, including dementia.
The Alzheimer's Society report indicates that expections for dementia care are low. While 68% of respondents feel the quality of care is good, only 41% feel the quality of life for the resident is good. The Alzheimer's Society report re-enforces other research findings that the level of activity for residents with dementia in care homes leaves room for improvement with only 41% saying opportunities for activity are good.
|
Care Quality Commission - 'Not Just a Number' - A national overview of the home care inspection programme
13 February 2013 |
The Care Quality Commission report 'Not Just a Number' reports on the results of a CQC inspection of a sample of 250 out of 6,830 registered home care agencies carried out from April 2012. These were agency office based inspections and there was no consistent attempt to capture the views of the person cared for or their relatives and friends.
Roughly three quarters (74%) of agencies met all five CQC standards in relation to respecting and involving people who use services, the care and welfare of care recipients, safeguarding care recipients from abuse, support for staff and the assessment and monitoring of service quality.
Key issues raised in the report included late and missed visits, a lack of consistency and continuity in care workers, a lack of support for staff and failure to address issues around travel time, poor care planning and a lack of regular reviews of care and poor staff understanding of their safeguarding and 'whistleblowing' responsibilities.
The report noted a reluctance, on the part of care recipients, to complain for fear of getting a regular carer into trouble or potential reprisals against the care recipient themselves.
A summary document and large print and easy read versions of the report are also available.
|
Government response to the Dilnot Commission proposals for the funding of social care in older age.
12 February 2013 |
The Government Policy statement on care and support funding reform accepts the principle of the Dilnot Commission proposals that there should be a maximum value for the social care costs that would need to be met by an individual in their life time.
The government proposals, most of which will not be implemented until April 2017, set the cap at £75,000 at 2017 prices compared with the Dilnot Commission suggested level of £35,000 (approx £43,000 at 2017 prices).
The proposals also increase the means-tested threshold beyond which financial help with residential care costs is no longer received from £23,250 to £123,000. The threshold for other types of care will be at an unspecified lower level.
The proposals apply only to care costs and exclude 'hotel' costs (food and accommodation) towards which someone in residential care will be expected to pay £12,000 annually (at 2017 prices). Care support payments will be at assessed fair and reasonable levels, rather than the actual cost of care, so full care costs will not necessarily be met.
A record of ongoing care costs towards the cap will be maintained in a 'Care Account' which is transferable between authorities.
|
The Francis Report - final report of the Mid Staffordshire NHS Foundation Trust Public Inquiry
6 February 2013 |
The final report of the Mid Staffordshire NHS Foundation Trust Public Inquiry chaired by Robert Francis QC, followed an earlier independent inquiry on the failings in the Mid Staffordshire NHS Foundation Trust between 2005 and 2009.
This final 'Francis Report' and the earlier inquiry report revealed a catalogue of failings in the care of older patients.
"There was a lack of care, compassion, humanity and leadership. The most basic standards of care were not observed, and fundamental rights to dignity were not respected. Elderly and vulnerable patients were left unwashed, unfed and without fluids. They were deprived of dignity and respect. Some patients had to relieve themselves in their beds when they offered no help to get to the bathroom. Some were left in excrement stained sheets and beds. They had to endure filthy conditions in their wards. There were incidents of callous treatment by ward staff. Patients who could not eat or drink without help did not receive it. Medicines were prescribed but not given. The accident and emergency department as well as some wards had insufficient staff to deliver safe and effective care. Patients were discharged without proper regard for their welfare."
The inquiry found "an institutional culture in which the business of the system was put ahead of the priority that should have been given to the protection of patients and the maintenance of public trust in the service".
The inquiry made a number of recommendations intended to achieve "a real change in culture, a refocusing and recommitment of all who work in the NHS - from top to bottom of the system - on putting the patient first".
|
ONS, release of ethnicity data from 2011 Census
11 December 2012 |
The first wave of Ethnicity data from the 2011 Census was released by ONS on 11th December 2012. The data revealed that, in 2011, just under one fifth (19.5%) of the population of England and Wales were from Black and Minority Ethnic groups. This was in line with CPA's projections in their report The Future Ageing of the Ethnic Minority Population of England and Wales, based on the 2001 census, which projected 21.4% by 2016. The latest data was included in a presentation by CPA's Nat Lievesley to the Runnymede / Age UK Ageing and Ethnicity Conference on December 13th which included CPA's projections of the ageing of the ethnic minority population, the incidence of dementia among BME groups and increases in the BME care home population.
|
Housing Learning and Improvement Network Resource Packs - "Hospital to Home" and "Strategic Housing for Older People"
26 October 2012 |
The Housing Learning and Improvement Network Hospital to Home Resource Pack contains essential information for all professionals that have a role in hospital discharge for older people in England. The pack, which aims to improve the integration of housing and support into the process for discharging older people, contains information, suggestions for action, case studies and checklists for considering older patients’ housing situations as part of hospital discharge and the transfer of care.
The Strategic Housing for Older People (SHOP) Resource Pack, helps with the 'Planning, designing and delivering of housing that older people want'. It is designed to help understand the current and future demand trends in housing with care and set out desired outcomes for local authorities and their partners.
|
Government White Paper "Caring for our future"
11 July 2012 |
The Department of Health has published Caring for our future, the government white paper on proposed changes to the care and support system.
The coalition government's proposed changes are said to be the most comprehensive overhaul of the care and support system since 1948.
The ‘Caring for our future’ White Paper sets out the vision for the reformed care and support system, the draft Care and Support Bill sets out social care legislation rationalising many statutes from the last 60 years, while the progress report on funding reform sets out the government’s position on social care funding.
Various organisations have published their responses and briefings to the White Paper including by Carers UK, part of the Care and Support Alliance, a policy briefing on the White Paper, along with briefings on the draft Care and Support Bill and the progress report on funding reform. See also, for example, the response from AgeUK.
|
Government Equalities Office response to its consultation on exceptions to age discrimination in the Equality Act 2010
12 June 2012 |
The Government Equalities Office has published its response to the consultation on exceptions to age discrimination in the Equality Act 2010.
The Government Equalities Office claim to have taken a proportionate approach, ensuring that the Equality Act 2010 prohibits only harmful or unjustifiable treatment that results in genuinely unfair discrimination and harassment because of or related to age.
The GEO has sought no exceptions in health and social care so all medical decisions based on age must be objectively justifiable. Financial services, on the other hand, have a blanket exception from the Act, although when age is used in decision making this must be made clear and, if cover is refused, signposts to alternative providers must be given.
Other exceptions include age based concessions, group holidays, immigration, sport, residential park homes and age verification schemes to control the purchase of age restricted products.
|
Health and Social Care Act (2012)
27 March 2012 |
On 27 March 2012 the Health and Social Care Bill gained Royal Assent to become the Health and Social Care Act (2012). This controversial act is likely to have a profound effect on the workings of the National Health Service. Supporters of the act argue that the act will deliver more power to clinicians, will put patients at the heart of the NHS, and will reduce the costs of bureaucracy. Opponents argue that it will lead to the fragmentation and marketisation of the health service.
|
Coalition Budget 2012
21 March 2012 |
The coalition government's 2012 budget delivered on 21st March 2012 included three key elements specifically affecting older people
- The phasing out of age related tax allowances from April 2013
- A statement of the intention to introduce a single tier state pension, above minimum income guarantee levels but based on contributions
- State pension age to be automatically reviewed as life expectancy improves
The most contentious budget proposal was the phasing out of age related tax allowances, introduced by Winston Churchill in 1925, in recognition of the financial pressures on older people. This additional allowance, for people aged 65 and over was a tapering allowance which became less as income increased and disappeared completely for incomes of £29,000 and above. The withdrawal of the allowance has been labelled by many commentators as a 'Granny Tax'.
The single tier state pension can be seen as part of a move towards a 'citizens pension', above means tested benefit levels, not based on contributions and is to be welcomed. The detailed implementation of this and any future 'citizens pension' will need careful consideration to avoid any sense of unfairness by older people who have made differing contributions and must also ensure that, after taking into account SERPS and S2P, no individual receives a lower state pension provision overall as a result of the measure.
Although it is desirable that increased longevity should result in older people spending a longer time in healthy and happy retirement, it has to be accepted as inevitable that the state retirement age should reflect improvements in life expectancy.
Further comment on the age related issues in the budget are available from Joseph Rowntree Foundation, National Pensioners Convention and Age UK.
|
The NHS Confederation, Age UK and the Local Government Association - Delivering Dignity - draft report for public consulation
29 February 2012 |
The NHS Confederation, Age UK and the Local Government Association established the Commission on improving Dignity in Care for Older People in July 2011 to identify the underlying causes of persistent failings and shortcomings in the care of older people.
A draft report recommending fundamental changes to the culture, leadership, management, staff development, clinical practice and service delivery of care homes and NHS hospitals was published for public consultation in February 2012.
The period of public consultation runs until Tuesday 27th March 2012.
|
Royal College of Psychiatrists - National Audit of Dementia
16 December 2011
|
The Royal College of Psychiatrists has published the full report and executive summary of its 2010 audit of dementia care in hospitals. The audit includes hospital policies and governance that recognise and support the needs of people with dementia, elements of comprehensive assessment, the involvement of carers, discharge planning, and identified changes to support needs during admission.
The audit highlights issues such as poor communication with families and a lack of personal care for patients. Patients with dementia tend to fare worse than other patients when they enter hospital and basic needs such as eating are often not properly attended to. There are issues with access to specialist services, and preparation for discharge from hospital through proper liaison with community services.
|
Equality and Human Rights Commission Report - Close to Home: An inquiry into older people and human rights in home care
23 November 2011 |
The Equality and Human Rights Commission has published both a full report and executive summary of it's inquiry into the human rights of older people receiving care at home.
Around half of the older people, friends and family members who gave evidence to the inquiry expressed real satisfaction with their home care but the inquiry revealed evidence that the poor treatment of many older people is breaching their human rights.
The inquiry highlighted a number of issues including:
- the low pay and status of care workers does not match the level of responsibility or the skills they need to provide quality home care.
- a high turnover of staff as a result of these factors has a negative impact on the quality of care given to older people.
- age discrimination is a significant barrier to older people getting home care.
- people over the age of 65 are getting less money towards their care than younger people with similar care needs, and are offered a more limited range of services in comparison.
- local authority phone contact lines can screen out older people needing home care without passing them on for a full assessment
Full details of the inquiry findings are available on the EHRC website.
|
Care Quality Commission to inspect Home Care companies
22 November 2011 |
The Care Quality Commission has announced that, from April 2012, it will inspect companies providing care (help with washing dressing etc) for elderly and disabled people in their own homes. This announcement is ahead of an Equality and Human Rights Commission report, due out on Wednesday 23rd November, which is expected to be critical of these services.
|
Care Quality Commission - National report on dignity and nutrition
13 October 2011 |
The Care Quality Commission has published its Dignity and nutrition inspection programme (DANI) National overview and reviews of individual NHS Trusts.
The report on Dignity and nutrition for older people, gives the findings of a series of 100 unannounced inspections of acute NHS hospitals in England between March and June 2011. The report reveals a catalogue of poor care and a need to change the culture on many wards with older people.
CQC checked two ‘outcomes’ during each inspection: Outcome 1, ‘respecting and involving people who use services,’ and Outcome 5, ‘meeting nutritional needs’. Of the 100 hospitals inspected:
- 45 hospitals met both standards (they were ‘fully compliant’).
- 35 met both standards but needed to improve in one or both (they were ‘fully compliant, with improvements suggested’).
- 20 hospitals did not meet one or both standards (they were ‘non-compliant, with improvements required’).
The problems often seemed to lie at ward level with variations between individual wards in the same hospital. CQC blame poor leadership with a culture of disrepect for patients being allowed to develop. CQC noted that one in five of its inspections had picked up care that posed risks to older people’s health and wellbeing.
|
The state of health care and adult social care in England
15 September 2011 |
The Care Quality Commission has published its annual review of state of health care and adult social care in England for 2010-11.
The report has four main sections dealing with: the shape of care provision; access to care and services; choice and control; and quality and safety. CQC note that, because of changes in the legal requirements for registration, it is not possible to make direct comparisons with figures about provision and capacity from previous years.
You can view the full report here or download the full report and summaries from the CQC website.
|
Caring for our future
15 September 2011 |
The Caring for Our Future engagement exercise aims to pinpoint the priorities that the Government needs to focus on to inform its formal plans to improve the care system. This consultation follows on from the report by the Dilnot Commission on Funding of Care and Support and the Law Commission report of its project to promote far-reaching reform of adult social care law.
The engagement exercise is led by a number of experts in the field:
- Quality - Imelda Redmond (Carers UK)
- Personalisation of Care - Jeremy Hughes (Alzheimer’s Society)
- Shaping local care services - Peter Hay (ADASS)
- Prevention - Alex Fox (NAAPS)
- Integration (in partnership with the NHS Future Forum) - Geoff Alltimes (Hammersmith and Fulham Council) and Dr Robert Varnam (Practising GP, Manchester)
- Role of financial services - Nick Kirwan (ABI)
...and will complete in December 2011.
|
Consultation on Dignity in Care
consultation closes
19 September 2011 |
The Commission on improving dignity in care - established as part of a joint initiative from the NHS Confederation, Age UK and the Local Government Group (LG Group), called Partnership on dignity in care - has been set up to improve dignity in care provided to older patients in hospitals and care homes.
The Commission is carrying out a consultation to gather evidence from people across health and socal care who understand the day to day pressures of providing care for older patients with complex needs. The consultation closes on 19 September 2011.
|
Dilnot Commission on Funding of Care and Support
04 July 2011 |
The Dilnot Commission has published Fairer Care Funding, its proposals for the future funding of the long term care of older people.
The commission's recommendations include
- no individual should pay more than £35,000 towards the health costs of their own long term care after which they would be eligible for full state support. This would, in adition, give individuals the opportunity to take out private insurance against a known risk.
- the present means tested income limit of £23,250, above which an individual has to pay for their own care, should be raised to £100,000.
- national eligibility criteria and portable assessments should be introduced to ensure greater consistency
- all those who enter adulthood with a care and support need should be eligible for free state support immediately rather than being subjected to a means test.
The Care and Support Alliance, a group of 26 charities of which CPA is a member, is supporting the commissions proposals
|
Equality and Human Rights Commission - Inquiry into home care of older people - interim findings
20 June 2011 |
The Equality and Human Rights Commission has published interim findings from its inquiry into home care of older people which reveal that older people’s basic human rights are being overlooked in the provision of care at home.
Major problems in the home care system that have been brought out by this inquiry include: inadequate time to deliver care; lack of control over timing of care visits; failure to deliver adequate homecare; lack of staff awareness and training; high staff turnover; low expections, passive acceptance and an unwillingness to complain on the part of care recipients.
The study has revealed a number of worrying cases including:
- people being left in bed for 17 hours or more between care visits
- failure to wash people regularly and provide people with the support they need to eat and drink
- people being left in soiled beds and clothes for long periods
- a high staff turnover meaning some people have a huge number of different carers performing intimate tasks such as washing and dressing. In one case a woman recorded having 32 different carers over a two week period.
|
Law Commission recommends reform of adult social care law
11 May 2011 |
The Law Commission has published the final report of its project to promote far-reaching reform of adult social care law.
The Commission's recommendation is for a single, clear, modern statute and code of practice that would pave the way for a coherent social care system. The intention is that older people, disabled people, those with mental health problems and carers will be clear about their legal rights to care and support services. Local councils in England and Wales will have clear and concise rules to govern when they must provide services.
The recommendations include putting the individual's wellbeing at the heart of decision-making, using new statutory principles; giving carers new legal rights to services; placing duties on councils and the NHS to work together; building a single, streamlined assessment and eligibility framework; protecting service users from abuse and neglect with a new legal framework, and giving adult safeguarding boards a statutory footing.
|
Consultation on the Government's proposals for simplifying the State Pension system
4 April 2011 |
The Government has launched a Consultation on its proposals for simplifying the State Pension system.
The consultation includes two options:
- to speed up the transition to a two tier flat rate pension; or
- to create a single tier flat rate pension above the Pension Credit standard minimum guarantee.
The consultation also seeks views on the most appropriate mechanism for determining future changes to State Pension age.
The consultation document is available as both pdf and rtf files, and a contact is provided for alternative formats.
The period of the consultation is from 4 April 2011 to 24 June 2011.
|
Analysis of The Law Commission's consulation on a legistlative framework for Adult Social Care
31 March 2011 |
The Law Commission has published an analysis of the responses to its consultation on a legislative framework to cover all aspects of Adult Social Care including assessment, eligibility for services, joint working and the safeguarding of vulnerable adults.
The analysis is available as a single document or in parts.
|
Review of statutory duties placed on local government
10 March 2011 |
The Department for Communities and Local Government is undertaking a comprehensive review of all statutory duties place on local government. Local Authorties are subject to many statutory duties in relation to older people including the duty to support frail older people in their own homes, to assess vulnerable people who appear to be in need and to co-ordinate appropriate care services to help them live as independently as possible,and the duty to carry out funerals for people who pass away alone, without any friends or family.
DCLG is seeking views on what duties are vital to keep, what duties should be repealed and what burdens have been created through particular duties, and associated regulations and guidance?
The informal consultation exercise will remain open for six weeks, closing 25 April 2011.
|
Independent Public Service Pensions Commission - final report
10 March 2011 |
The Independent Public Service Pensions Commission, chaired by John Hutton (Lord Hutton of Furness), has published its final report on public service pension provision setting out its recommendations to the Government on pension arrangements that it believes are sustainable and affordable in the long term, fair to both the public service workforce and the taxpayer and consistent with the fiscal challenges ahead, while protecting accrued rights.
|
Department of Health
Paul Burstow announces DH will not seek any exceptions to the Equalities Act 2010 for Health and Social Care
03 March 2011 |
"The NHS must never discriminate based on age" was the message given by Care Services Minister Paul Burstow announcing that the Department of Health will not be seeking any exceptions to the planned implementation of the Equality Act 2010.
"As part of its commitment to a personal, fair and diverse service that protects patients’ dignity and ensures that all patients receive the best possible treatment regardless of their age, the Department of Health will not be seeking any exceptions."
|
Government Equalities Office
Consultation on exceptions to the Equalities Act 2010
03 March 2011 |
The Government has commenced a consultation in relation to age discrimination in the provision of services and public functions.
The consultation 'Equality Act 2010: Banning age discrimination in services, public functions and associations - A consultation on proposed exceptions to the ban' sets out the specific exceptions where the government believes that different treatment of people of various ages is justified or beneficial and where legislation will help clarify that these practices can continue; and proposes how the legislation will be drafted to take account of these.
A link to the consultation document and other supporting information can be found on the Government Equalities Office website.
|
Care and Compassion?:
Report of the Health Service Ombudsman on ten investigations into NHS care of older people
14 February 2011 |
'Care and Compassion?', a report presented to Parliament by the Health Service Ombudsman for England, Ann Abraham, describes ten investigations into complaints about the standard of care provided to older people by the NHS.
The complaints were made about NHS Trusts across England, and two GP practices. Each investigation was conducted independently in 2009 and 2010 and collated together because of the common experiences of the patients concerned and, as the Ombudsman states, because of the stark contrast between the reality of the care they received and the principles and values of the NHS. The findings show that the reasonable expectation that an older person or their family may have of dignified, pain-free end of life care, in clean surroundings in hospital, is not being fulfilled. The investigations reveal an attitude - both personal and institutional - which fails to recognise the humanity and individuality of the people concerned and to respond to them with sensitivity, compassion and professionalism.
Printable (pdf) version.
|
No health without mental health: a cross-government mental health outcomes strategy for people of all ages.
2 February 2011 |
This cross Government mental health outcomes strategy No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages sets out six shared objectives to improve the mental health and well-being of the nation, and to improve outcomes for people with mental health problems. It takes a life course perspective covering children to young adults, adults to older people in order to:
- improve the mental health and wellbeing of the population and keep people well, and
- improve outcomes for people with mental health problems through high quality services that are equally accessible to all.
The aim is to mainstream mental health so that it becomes as important to people as their physical health. Key to reducing the estimated £105 billion annual cost of mental ill-health to the economy is to intervene early to stop problems developing and to prevent illness through public mental health and well-being actions across the board.
|
Health and Social Care Bill 2011
19 January 2011 |
The Health and Social Care Bill, introduced into Parliament on 19 January 2011, is a crucial part of the Government's vision to modernise the NHS so that it is built around patients, led by health professionals and focused on delivering world-class healthcare outcomes.
The Bill takes forward the areas of Equity and Excellence: Liberating the NHS (July 2010) and the subsequent Government response Liberating the NHS: legislative framework and next steps (December 2010), which require primary legislation. It also includes provision to strengthen public health services and reform the Department's arm's length bodies.
The Bill contains provisions covering five themes:
- strengthening commissioning of NHS services
- increasing democratic accountability and public voice
- liberating provision of NHS services
- strengthening public health services
- reforming health and care arm's-length bodies.
|
End of the line for the default retirement age
13 January 2011 |
The Government confirmed that it will remove the Default Retirement Age (DRA) so that people have more choice when to stop working. The Government claim that, as well as benefiting individuals, the freedom to work for longer will provide a boost to the UK economy.
Ministers have decided to proceed with their plan to phase out the DRA between 6 April and 1 October 2011. The Government's written response to its recent consultation on the issue, and new ACAS guidance to help businesses adapt to the removal of the regulation, have also been published.
Currently the DRA enables employers to make staff retire at 65 regardless of their circumstances, but the Government feels the rules must change as people are living longer, healthier lives.
|
Liberating the NHS: Legislative framework and next steps
14 December 2010 |
Liberating the NHS is the government's response to the consultation period following the launch of the white paper Equity and Excellence: Liberating the NHS published in July 2010. In this response the Government sets out the next steps and timetable in its plan to reform the NHS and announces that £89 billion will go direct to PCTs for frontline services - equivalent to a 3% increase in funding for the NHS. The reforms are designed to put patients at the heart of the NHS. Also published are the PCT Allocations and NHS Operating Framework for 2011/12.
The Operating Framework sets out what NHS organisations must focus on in 2011/12 to prepare for transition to the new system of GP commissioning and includes:
- the need to continue to improve performance, for example on waiting times
- Primary Care Trusts (PCTs) streamlined into clusters, working with GP practices and emerging GP consortia on commissioning as well as reducing running costs
- the role of the NHS Commissioning Board, which will operate in shadow form from next year to ensure an efficient and effective transition.
To date 52 GP consortia have signed up as pathfinders to manage their local budgets and commission services for patients. In total, the pathfinders involve 1860 GP practices and cover around 25% of the population - some 12.8 million people.
|
The Localism Bill
13 December 2010 |
The Localism Bill contains a package of reforms designed to devolve greater power and freedoms to councils and neighbourhoods, establish new rights for communities, change the planning system and give communities control over housing decisions. The Government's intention is that the legislation will help build the Big Society by radically transforming the relationships between central government, local government, communities and individuals.
Summary of the Bill: To make provision about the functions and procedures of local and certain other authorities; to make provision about the functions of the Local Commission for Administration in England; to enable the recovery of financial sanctions imposed by the Court of Justice of the European Union on the United Kingdom from local and public authorities; to make provision about local government finance; to make provision about town and country planning, the Community Infrastructure Levy and the authorisation of nationally significant infrastructure projects; to make provision about social and other housing; to make provision about regeneration in London; and for connected purposes.
The Government has today also published Decentralisation and the Localism Bill: an essential guide. Its sets out six actions central government will need to take to achieve and maintain the radical shift in power, - in behaviour, expectation, and culture - which must go alongside the changes in law proposed in the Bill. |
Healthy lives, healthy people: our strategy for public health in England
30 November 2010
Deadline for responses to consultation March 8th 2011 |
The public health White Paper 'Healthy lives, healthy people' casts the Government's long-term vision for the future of public health in England, aiming to create a 'wellness' service, a new integrated public health service, (Public Health England) and to strengthen both national and local leadership. It responds to Professor Sir Michael Marmot's Fair Society, Healthy Lives report and adopts a life course framework for tackling the wider social determinants of health. The aim is to build people's self-esteem, confidence and resilience right from infancy - with stronger support for early years. It complements A Vision for Adult Social Care: Capable Communities and Active Citizens in emphasising more personalised, preventive services that are focused on delivering the best outcomes for citizens and that help to build the Big Society. There is a specific focus on ageing well (see e.g. p47-50).
The White Paper includes consultation questions - the closing date is March 8th 2011. |
Recognised, supported and valued: Next Steps for the 'Carers Strategy'
25 November 2010 |
This is a cross-government document setting out how the government will prioritise actions over the next four years to ensure the best possible outcomes for carers and those they support. The strategy identifies the actions that the Government will take to support these priorities. These include: (1) providing £400m additional funding over the next four years for breaks, and further resources for GP training, to increase GPs’ awareness and understanding of carers’ needs for support; (2) the Department for Education will make a new early intervention grant available to local government from April 2011-12, bringing together a range of funding streams for early intervention services for young people and families, including young carers; (3) the Department for Business, Innovation and Skills will issue a consultation document next year to consult with business on how best to take forward the Coalition commitment to extend to all employees the right to request flexible working;
(4) the Department of Health and the Department for Business, Innovation and Skills will examine how small local enterprises can be encouraged to provide good quality, reliable and consistent replacement care either to give carers a break from caring responsibilities or to enable them to work alongside caring responsibilities; and
(5) the Department of Health and the Department for Business, Innovation and Skills will work with industry and statutory and voluntary sector stakeholders to identify the barriers and enablers to market growth in assisted living technologies, and to support further uptake and boost innovation.
Read the Carers Strategy here.
|
|
Carers and Personalisation: Improving Outcomes
Department of Health |
The Department of Health has produced a guide exploring personalisation in relation to carers, Carers and Personalisation: Improving Outcomes. It presents emerging evidence with examples to illustrate how the principles of personalisation have been applied, emphasising the value of finding ways forward that make sense and work best locally. Read the evidence guide here.
|
Local Delivery of Joined-Up Services
Department for Work and Pensions
24 November 2010 |
This research builds on the lessons of LinkAge Plus in looking at other Local Authority areas that had developed a similar approach to joining-up services or adopting similar principles to LinkAge Plus. Some of these were influenced directly, e.g. Lancashire County Council has taken forward many of the principles of the LinkAge Plus pilot in Lancaster. Others have come to many of the same principles of LinkAge Plus in different or innovative ways. Drawing on case study participants’ experience, a framework has been developed for implementing and sustaining more joined-up working.
Read the research and case studies here. |
The Forgotten Age: Understanding Poverty and Social Exclusion in Later Life (Interim Report)
The Centre for Social Justice
23 November 2010 |
The Forgotten Age documents levels of poverty and social exclusion facing many people in older age challenged in terms of money, health, lifestyle, communities, housing and care. The report identifies two key threats to the well-being of older people - the crisis in social care where demand is set to rise sharply against the background of continuing public spending constraints, the absence of any clear policy remedy from government and a projected severe fall in the number of unpaid carers currently looking after millions of vulnerable old people; and the high and rising levels of family breakdown is impacting the old as well as the young, meaning that in the future fewer old people will have adult children and spouses and partners to turn to when they need help with the simple essentials of everyday life, such as washing, dressing, travelling to the shops and cooking.
Read The Forgotten Age here and access background information via the Centre for Social Justice website. |
A Vision for Adult Social Care: Capable Communities and Active Citizens
Department of Health
16 November 2010
|
The vision sets out a new agenda for adult social care in England that provides more control to individuals and their carers. It is built on seven principles: Prevention; Personalisation; Partnership; Plurality; Protection; Productivity; and People.
Reform of the system of social care in England focuses on the government commitment to:
- break down barriers between health and social care funding to incentivise preventative action in local communities
- extend the greater rollout of personal budgets to give people and their carers more control and purchasing power;
- use direct payments to carers and better community-based provision to improve access to respite care.
- encourage care and support to be delivered in a partnership between individuals, communities, the voluntary sector, the NHS and councils - including wider support services, such as housing.
Launching the vision, Paul Burstow, Minister for Care Services, announced that everyone eligible will receive a personal budget, preferably as a direct payment, by 2013.
Read A Vision for Adult Social Care here.
|
Transparency in Outcomes: A Framework for Adult Social Care
A Consultation on Proposals,
16 November 2010-9 February 2011.
|
This consultation document proposes a new strategy for transparency, quality and outcomes in adult social care. It sets out an enabling framework which aims to empower councils, local people and the wider social care sector to take new leadership roles. It provides a support to the critical link between adult social care and other local partners, such as the NHS, as well as demonstrating social care’s important contribution to the Government’s new Transparency Framework. The document includes specific questions as part of the consultation and the government will publish its response by April 2011.
Read the consultation document here. |
Inquiry into Home Care of Older People
Equality and Human Rights Commission (EHRC)
Launched 10 November 2010
|
The EHRC has begun an Inquiry into the protection and promotion of human rights of older people in England who require or receive home-based care and support.
The inquiry will investigate the experiences of, and as a result confidence in, the system to protect human rights of older people and their families. It will explore the legal obligations of different groups, including care providers, local authorities, the Care Quality Commission and central government.
It will specifically look at whether obligations are being discharged effectively in the context of reforms to the care and support system and evidence of good practice in this area. Finally the Inquiry will look at the case for legislative reform to ensure that the human rights of vulnerable older people are comprehensively and robustly protected.
The Inquiry will publish its findings and recommendations in December 2011.
A Call for Evidence is asking for good or unsatisfactory experiences of homecare from older people, their family and friends and from home care staff and organisations.
Access Inquiry details and how to contribute to the call for evidence via the EHRC website here. |
Think Local, Act Personal: Next Steps for Transforming Adult Social Care
4 November 2010 |
Think Local, Act Personal is a proposed sector-wide partnership agreement to moving forward with personalisation and community based support. The agreement draws on learning from implementing Putting People First across England over the past three years and focuses on areas where further action is required. The agreement: (1) Underlines the necessary connection between preventative, community-based approaches and personalised care and support; and (2) Provides a general framework for action; supported in the next few months by examples to assist partners in benchmarking progress, and by co-designed tools to aid delivery.
Read Think Local, Act Personal here.
|
Universal Credit: Welfare That Works, White Paper,
Department for Work and Pensions
11 November 2010
|
Secretary of State for Work and Pensions, Iain Duncan Smith announced today welfare reforms moving towards a universal credit intended to replace work-related benefits and simplify the benefits system.
He proposed a 'comprehensive system of support' to help people back into employment, and sanctions for those who refuse to take up work offered.
The new Credit will provide a basic amount with additions for those with children and other caring responsibilities, people with disabilities and those with housing needs. It will be available for people both in and out of work and will replace the existing support including: Working Tax Credit, Child Tax Credit, Housing Benefit, Income Support, income-based Jobseeker’s Allowance and income-related Employment and Support Allowances. Read the White Paper here and the Executive Summary here. |
| An Age Old Problem
National Confidential Enquiry into Patient Outcome and Death (NCEPOD)
11 November 2010 |
This new study from NCEPOD investigated all the deaths of patients over 80 that took place in hospitals within 30 days of surgery over a three-month period of 2008, questioning medical staff and examining case notes. Less than one third of patients (225/965) were reviewed by specialist elderly care teams before surgery. 'Most patients were admitted as emergencies by very junior doctors without timely input of senior care of the elderly clinicians.' Read the full report here.
Key findings
• Just over 1/3 of patients surveyed (38%, 295/786) received good care.
• Poor nutrition and serious associated illness were very common in the group
studied.
• In over two-thirds of cases (67.7%, 653/965), patients were not reviewed by
specialists in Medicine for the Care of Older People.
• Clinically significant delays occurred in 1 in 5 patients between admission and
their operation.
• 1/4 of hospitals had no acute pain service.
See the Centre for Policy on Ageing's reviews on age discrimination in health and social care services. |
Independent Public Service Pensions Commission chaired by Lord Hutton
Call for evidence 1 November-17 December 2010 |
Lord Hutton has issued a call for evidence to feed into his final report on restructuring public service pensions, due to be published before Budget 2011. The Call asks specific questions around design of pension scheme, risk-sharing and adequacy. Read the Call for Evidence here. |
Financial Management of Personal Budgets: Challenges and Opportunities for Councils
Audit Commission
28 October 2010 |
In May 2010, the Coalition Government re-stated its commitment to personal budgets. This report reviews progress of people taking control of their own social care. It fnds that some councils are falling behind in providing personal budgets and will need to make 'a significant effort' to achieve the milestones agreed in 2009 between the Association of Directors of Adult Social Services, the Local Government Association and Department of Health that at least 30 per cent of eligible social care users, or their carers, should have a personal budget by April 2011. Only six of the 152 councils are currently meeting it. In addition, a survey earlier in 2010 showed only 6% of total spending on adult social care had so far been allocated to personal budgets.
The report also reveals that councils have less well-developed personal budget approaches for people with mental healthcare needs. Several did not provide them at all, despite evidence that mental health service users would be major beneficiaries of the policy. It suggests that existing joint arrangements are not flexible enough to adapt to personal budgets.
Read the full report and summary report. |
HM Treasury Spending Review
20 October 2010 |
Full details of the comprehensive spending review can be accessed here.
The Spending Review confirms key components of the Coalition Agreement setting out the Government’s objectives and priorities for the Parliament, including commitments to:
•• provide an NHS that is free at the point of use and available to everyone based on need not the ability to pay, with total NHS spending increasing in real terms in each year of the Parliament;
•• uprate the basic State Pension by a triple guarantee of earnings, prices or 2.5 per cent, whichever is highest, from 2011, while bringing forward the date at which the State Pension Age will start to rise to 66 to 2018 in order to ensure this is fiscally sustainable.
Section 1.63. Key benefits for older people:
“The Government is preserving key benefits for older and vulnerable people, including Winter Fuel Payments, free eye tests, prescriptions and TV licences. In addition, the Government will:
•• allocate £2 billion of additional funding a year by 2014-15 to social care to support some of the most vulnerable people in society;
•• make permanent the temporary increases to Cold Weather Payments provided in the past two winters, at a cost of £50 million a year, so that eligible households receive £25 for each seven day cold spell recorded or forecast where they live; and
•• protect the statutory entitlement for concessionary bus travel, ensuring that older people can maintain greater freedom and independence.” |
Building a Stronger Civil Society: A strategy for voluntary and community groups, charities and social enterprises
14 October 2010
Deadline for responses to consultation 6 January 2011 |
Together with citizens and communities, the voluntary and community sector sits at the heart of the government's ambitions to create a Big Society. Proposed reforms will re-caste the relationship between the state and the sector, giving it opportunities to shape and provide innovative, bottom-up services where state services have failed. The strategy outlines the sector's potential role in empowering communities, opening up public services and promoting social action. It highlights a range of existing policies and some new initiatives for supporting civil society organisations at a challenging time. Read the strategy here.
As part of this new strategy, the Government has launched a consultation in which it is seeking views on how it can improve the effectiveness of the advice and support that is available to frontline organisations. Read the consultation document here. |
21st Century Welfare
DWP
30 July 2010
Consultation 30 July-1 October 2010 |
The DWP discussion document provides a framework to reform the benefits system, maximising work incentives while continuing to protect those most in need. The proposals for a simpler benefit system could: bring together parts of the current benefits and tax credit syste; simplify the financial help available to people both in and out of work; and allow extra support for housing, children and disability. A consultation paper on changes proposed ran from 30 July until 1 October 2010. Read the full document and summary here. |
Phasing Out the Default Retirement Age: Consultation Document,
29 July 2010
Deadline for responses
21 October 2010
|
The government is committed to phasing out the default retirement age (DRA). The consultation document sets out the background to the DRA and explains how the government is proposing to remove it. Reasons given for removing the DRA include demographic change; the financial benefits to the individual and the wider economy; and the health and social benefits people gain from working later in life. The consultation asks questions on the specific proposals the government has for phasing out DRA and on the support individuals and businesses might need to manage in its absence. Deadline for receipt of responses is 21 October 2010. Read the consultation document here. Access futher information from the Department of Business Innovation and Skills website. |
Commission on the Funding of Care and Support
20 July 2010
|
The Commission on the Funding of Care and Support set up by Health Secretary Andew Lansley will 'make recommendations on how to achieve an affordable and sustainable funding system for care and support, for all adults in England, both in the home and other settings. The Commission should build on the extensive existing body of work in this area and provide advice on how to implement its chosen option.' Andrew Dilnot is chair of the Commission; two other Commissioners are Dame Jo Williams and Lord Norman Warner. The Commission wants to work with all users of care and support, the public, stakeholders and experts. The focus is on working collaboratively with all stakeholders and to gather the evidence, input and advice of others. This will be through an external reference group and by drawing on the expertise of two expert independent panels, one comprising of academics and the other of experts drawn from the financial services industry. The Commission is to present its findings to the government by the end of July 2011.
Further details on the terms of reference of the Commission, the Commissioners and reasons for reform are given on the DH website - click here to access
|
Call for Evidence on the future funding of care and support
1 December 2010
Deadline for responses
28 January 2011
|
The Call for Evidence paper seeks suggestions on the future funding of care and support in England and forms one part of the wider engagement work - click here to access |
Equity and Excellence: Liberating the NHS
DH White Paper
12 July 2010
A consultation on proposals was launched on 18 October, closing on 14 January 2011
|
The White Paper sets out the government's long-term vision for the future of the NHS. It asserts patients will have greater choice and control including a focus on personalised care that reflects individuals' health and care needs, supports carers and encourages strong joint arrangements and local partnerships. Access the White Paper and supporting documents here.
The NHS will focus on outcomes and the quality standards that deliver them to improve patient experience. Reforms are intended to empower professionals and providers, giving them more autonomy and making them more accountable to the public at local level. In particular, power and responsibility for commissioning services will be devolved to GPs and their practice teams working in consortia. To achieve savings for reinvestment in front-line services the NHS will need to cut bureaucracy and improve efficiency.
The role of the DH itself will change. Its NHS role will be reduced and it will focus more on strategy to improve public health, tackle health inequalities and reform adult social care. More powers around public health improvement will be transferred to local authorities. Read the consultation document.
The DH will maintain its vital role in setting adult social care policy to provide a sustainable system that gives people support and freedom to live with dignity. It will seek to break down barriers between health and social care funding to encourage preventative action. The government's vision for social care will be set out later in 2010 (published November 2010, see above). The DH will establish a commission on the funding of long-term care and support to report within a year. The government will bring together the conclusions of the Law Commission and the Commission on funding of long-term care, along with its vision, into a White Paper in 2011, with a view to introducing legislation in the second session of this Parliament to establish a sustainable legal and financial framework for adult social care. |
Ageing Well programme launched by DWP on 12 July 2010 |
Ageing Well is a new programme designed to support local authorities to improve their services for older people. The key aim of the programme is to provide a better quality of life for older people through local services that are designed to meet their needs and recognise the huge contribution that people in later life make to their local communities. It is a sector led programme which consolidates current best practice from local authorities, the findings of wider research and the lessons learned from earlier pilot activities. This combined body of evidence shows that strong leadership, working in partnership, joining up services and including older people in service design and delivery, leads to more cost effective services with better outcomes for older people. |
Two Reviews on Pensions announced 24 June 2010
Increasing the state pension age to 66
Enrolment into workplace pensions |
The coalition government announced two reviews on pensions on 24 June 2010.
A review has been established into the timing of the increase in state pension age to 66. A Call for Evidence is inviting people and organisations to submit evidence on the following:
· Changes in life expectancy and the changed economic context
· The notice period for individuals affected
· Ensuring no group is disproportionately impacted
The Call closed on 6 August and the Government response to the call for evidence was published 3 November 2010 - click here to read.
The second review focused on how best to support the implementation of automatic enrolment into workplace pensions, reporting by end September 2010 (panel: Paul Johnson; David Yeandle OBE; Adrian Bolding). On 27 October 2010 the Government published the outcomes of the independent review into how to make automatic enrolment work - click here to read.
Access further information via the DWP's website.
The government is restoring the link between the state pension and earnings from 2011 and consulting on how to phase out quickly the Default Retirement Age.
|
Independent Public Service Pensions Commission
Chaired by Lord Hutton
June 2010
Interim report published 7 October 2010
|
Ex-Labour cabinet minister John Hutton has been appointed to head a commission into public sector pensions. The commission will undertake a fundamental structural review of public service pension provision by Budget 2011. It will produce an interim report in September 2010 ahead of the Spending Review. The Commission is extending an invitation to all interested groups to submit their views and comments directly and has requested all responses by end July 2010. Access the terms of reference here
An interim report was produced on 7 October outlining progress to date on undertaking a structural review of public service pensions. Read the report. |
Social Care Commission announced in the Queen's Speech 25 May 2010 |
'The government recognises that urgent reform of the social care system is needed to provide much more control to individuals and their carers, and to ease the cost burden that they and their families face. This is one of the biggest challenges faced by society today. The government will establish an independent Commission to consider how we ensure responsible and sustainable funding for long-term care. It will ensure that there is a fair partnership between the state and the individual, which takes into account the vital role of families and carers. The commission will report within a year.' |
The Personal Care at Home Act
8 April 2010 |
The Personal Care at Home Act amends section 15 of the Community Care (Delayed Discharges etc.) Act 2003 so as to remove the restriction on the period for which personal care may be provided free of charge to persons living at home; and to make consequential provision.
Both Houses of Parliament have to approve implementation of the measure in a vote and the coalition government has announced that it will not be commencing the provisions in the Act relating to free care at home. |
The Equality Act 2010
8 April 2010 |
The Equality Act is due to come into force in October 2010, with the public sector equality duty due to come into force on April 2011 and age protection outside the workplace in April 2012. Access further details via the Government Equalities Office (GEO) website. |
Building a National Care Service - White Paper
30 March 2010 |
The Labour government proposed fundamental reform of the care and support system for all adults in England building a new National Care Service.
Read the White Paper and supporting documents here. |
Reshaping Care for Older People
The Scottish Government,
24 March 2010
|
Reshaping Care for Older People engages all sectors in a programme to explore how older people's care can be delivered over the next two decades. If current models of care in Scotland are sustained, the present care budget of £4.5 billion will need to rise by £1.1 billion by 2016 and £3.5 billion by 2031. In partnership with Scotland's local authorities and involving the voluntary and private sectors, the programme will include a series of public meetings around Scotland to share the future challenges and possible solutions with a wide audience. There are eight primary work streams. Access developments through the Scottish Government website here. |
Securing Good Care for More People: Options for Reform
The King's Fund (Richard Humphries, Julien Forder, Jose-Luis Fernandez)
16 March 2010 |
In light of changing circumstances and increasing demand for social care, this report takes forward the 2006 review of social care by the King's Fund (Wanless report) to provide fresh evidence of the 'compelling need for reform' with projections drawing on revised modelling. The analysis looks at three funding options over 2015-2026: the existing system with no reform; free personal care; and a revised version of the partnership model put forward in the original review in which the state funds 50% of everyone's care and support costs, and matches every £2 contributed by the individual with a further £1. A key principle of reform is that costs of care need to be shared responsibly between the individual and the state. While each option modelled calls for an increase in public funding, the report suggests a revised version of the original partnership model offers the best outcomes. Read the full report here. |
Social Care: Third Report of Session 2009-10
House of Commons Health Committee
12 March 2010 |
The House of Commons Health Committee report on adult social care provides a wide ranging analysis of the current status of social care, shortcomings of the existing system and requirement for fundamental and lasting reform. The Committee cautions against creating an atmosphere of 'demographic despair and alarmism' in the face of changing demographics as society must not underestimate its ability to be productive and create wealth, nor underestimate the contribution of older people. However, in the face of unmet need, increased demands and perceived unfairness in people accessing social care support, the Committee calls on all political parties to come together to map out sustainable reform. Read the full report here or browse through individual sections here. |
Age Equality in Health and Social Care: A Report on the Consultation
Department of Health
9 March 2010 |
This is a report on the consultation that the DH conducted from November 2009 to February 2010 on age equality in health and social care. It summarises responses to questions and details the position of the DH on each issue and further actions. Annex A of the report provides a summary of the DH position in relation to specific issues, including timing of the ban on age discrimination, exceptions, QALYs, upper limit for the breast screening programme, age specific datasets, and more. Read the full report, summary document and original consultation questions here. |
Law Commission, Adult Social Care: Consultation
24 February - 1 July 2010 |
The Law Commission, which advises the Government on law reform, has proposed to replace existing laws and policy guidance for adult social care with a single, modern statute in England and Wales. The legislative framework for adult residential care, community care, adult protection and support for carers is inadequate, often incomprehensible and outdated. Provisional proposals include:
• establishing a core set of overarching principles to guide social care decisions;
• introducing a single and explicit duty to assess individuals’ needs;
• a duty on local authorities to provide community services for all those eligible;
• the introduction of a single duty to assess the needs of any carer;
• a statutory duty on local authorities to investigate when they suspect that
vulnerable adults are being abused or neglected.
Read the consultation paper and related information here. The Commission has agreed to publish the final report by April 2011. |
Under Pressure: Tackling the Financial Challenge for Councils of an Ageing Population
Audit Commission
18 February 2010 |
The Audit Commission report on local government examines the issues facing councils with an ageing population requiring a range of services as public spending reduces. It suggests that councils are not planning strategically for an ageing population and do not know enough about the costs. In addition, cost savings that could arise from preventive services and better work with other organisations are not being explored fully by councils.
Read the summary report, full report and associated documents here. |
Fair Society, Healthy Lives
The Marmot Review
11 February 2010 |
The aim of the Review was to propose an evidence based strategy for reducing health inequalities from 2010. The strategy includes policies and interventions that address the social determinants of health inequalities.The starting point for the Review is that health inequalities that are preventable by reasonable means are unfair, and putting them right is a matter of social justice. Key messages from the Review include: there is a social gradient of health - the lower a person's social position, the worse his or her health. Action should focus on reducing the gradient in health. Health inequalities result from social inequalities. Action on health inequalities requires action across all the social determinants of health. Universal action is required but with a scale and intensity that is proportionate to the level of disadvantage - called 'proportionate universalism'. The fair distribution of health, wellbeing and sustainability are important social goals. Read the Executive Summary here. Access the full report and supporting documents here. |
The State of Health Care and Adult Social Care in England: Key themes and quality of services 2009
Care Quality Commission
10 February 2010 |
The Care Quality Commission (CQC) published its first report annual report to Parliament on the state of health care and adult social care in England. The future presents a major challenge with increasing demand for care at a time when public finances will be stretched. The CQC calls for faster progress in joining up health and social care with better care in the community. Also a fundamental cultural shift is required to enable people to have more choice and control over their care. This includes providing better information about care options, widening access to care and challenging discrimination and promoting human rights within services. Read the full report here. Access a summary of the report and further information from the CQC here. |
Equality Bill: Making it work. Policy proposals for specific duties
Ending age discrimination in services and public functions
25 and 27 January 2010 |
The Government Equalities Office (GEO) published two policy statements relating to work around proposed implementation of the Equality Bill.
'Policy proposals for specific duties' provides the response to the consultation on proposals for the specific equality duties and 'Ending age discrimination in services and public functions' summarises the consultation responses and sets out plans for specific exceptions from the age discrimination ban. The GEO is requesting feedback on whether to create specific exceptions around age for health and social care within the legislation, with the request to send comments by 30 April 2010 to age@geo.gsi.cog.uk as noted in the policy statement. Read the Centre for Policy on Ageing's response on exceptions and related issues here. |
National Evaluation of Partnerships for Older People Projects: Final Report
18 January 2010 |
The Partnership for Older People Projects (POPP) were funded by the Department of Health to develop services for older people, aimed at promoting their health, well-being and independence and preventing or delaying their need for higher intensity or institutional care. The evaluation found that a wide range of projects resulted in improved quality of life for participants and considerable savings, as well as better local working relationships. Read the executive summary here or access the full report via the DH website here. |
Four reviews from the literature on ageism and age discrimination in secondary health care, primary and community health care, mental health care and social care in the United Kingdom
Centre for Policy on Ageing
21 December 2009 |
The Centre for Policy on Ageing published on 21 December 2009 four reviews from the literature to provide evidence of ageism and age discrimination in primary and community health care, secondary health care, mental health care and social care in the UK. Access the four reviews via the CPA website here.
The four reviews were commissioned by the Department of Health to support the national review of age discrimination and age equality in the health and social care sector and help health and social care organisations meet the new public sector equality duty in the Equality Bill.
This recent work complements earlier work consisting of two literature reviews and two research studies on the costs and benefits of eliminating age discrimination in the provision of health and social care commissioned by the Department of Health and released on 26 June 2008 to coincide with the launch of the first draft of the Equality Bill in the House of Commons.
The review of the likely costs and benefits of legislation to outlaw age discrimination in health and social care was carried out by the Centre for Policy on Ageing. View the CPA report | Link to all four reports on DH website
|
The Personal Care at Home Bill
25 November 2009 |
The Personal Care at Home Bill, announced in the Queen's Speech on 18 November, was introduced to Parliament on 25 November 2009. The Bill offers free personal care at home for those with the highest needs, regardless of means, such as those with serious dementia and with Parkinson's Disease. It includes provision to invest in re-ablement and prevention to help people live at home for longer. |
Achieving Age Equality in Health and Social Care
A Report to the Secretary of State for Health by Sir Ian Carruthers OBE and Jan Ormondroyd
22 October 2009
|
The national review of age discrimination and age equality in the health and social care sector was set up to help health and social care organisations meet the ban on age discrimination and the new public sector equality duty in the Equality Bill. The review analysed evidence about the nature, extent and variability of age discrimination in health and social care services. Read the report of the national review here. An annex of working papers to support 'Achieving Age Equality in Health and Social Care' is available to read here.
The DH commissioned a resource pack including audit tools and practice guides, to be available from April 2010, to assist with the elimination of ageist and discriminatory practice at local levels. |
Shaping the Future of Care Together -Green Paper
14 July 2009
|
The Green Paper set out the Labour government's vision for a new care and support system based on a National Care Service that is fair, simple and affordable. It outlines six elements that people should be able to expect from the new service: prevention services; national assessment; a joined-up service; information and advice; personalised care and support; and fair funding. Three key changes are required to help meet these six objectives: more joined-up working; a wider range of services in care and support; and better quality and innovation. To read the Green Paper click here. A national debate on the reform of adult care and support in England - the Big Care Debate - closed on 13 November 2009. |
Building a Society for All Ages
13 July 2009
Response to consultation published 2 Feb 2010 |
Building a Society for All Ages builds on the cross-government Opportunity Age strategy to meet the challenges and realise the opportunities of an ageing population. To read the report click here. The government invited views on proposals to continue this work as part of a formal consultation process. The consultation questions and reports supporting the strategy, including the final report Working Together for Older People in Rural Areas, are available via the government website - click here to access. Read the consultation response report here. |
National Review of Age Discrimination in Health and Social Care
May - October 2009 |
A national review of the actions required to implement the provisions in the Equality Bill relating to age discrimination in health and adult social care was led by Sir Ian Carruthers, Chief Executive of the South West Strategic Health Authority, and Jan Ormondroyd, Chief Executive of Bristol City Council. |
The Equality Bill
Introduced 24 April 2009 - Completed 7 April 2010 |
The Equality Bill had its First Reading on 24 April 2009. Age discrimination was banned in the workplace in 2006 and the Equality Bill will make it unlawful to discriminate against someone aged 18 or over because of age when providing services or carrying out public functions. It will not affect products or services for older people where age-based treatment is justified or beneficial. The law will only stop age discrimination where it has negative or harmful consequences. The new law will be implemented in phases, with main provisions in October 2010 and the ban on age discrimination in provision of goods, facilities, services and public functions in 2012. The government has initiated a review of the practical action that is needed to tackle age discrimination in health and social care, which will report in October 2009. Access the Equality Bill and associated documents here. |
Living Well with Dementia: A National Dementia Strategy
Department of Health
3 February 2009
The NDS Joint Commissioning Framework (added 15 June 2009)
Dementia Gateway
The Use of Antipsychotic Medication for People with Dementia: Time for action
12 November 2009 |
The first National Dementia Strategy sets out initiatives designed to improve the lives of people with dementia, and their carers and families. The Strategy aims to increase awareness of dementia, ensure early diagnosis and intervention and radically improve the quality of care that people with the condition receive. Proposals include the introduction of a dementia specialist into every general hospital and care home and for mental health teams to assess people with dementia, with memory clinics to be established throughout England. To read the National Dementia Strategy click here. The strategy draws on the results of a public consultation.
The NDS Joint Commissioning Framework, a new resource to support implementation of the National Dementia Strategy, provides best practice guidance for commissioning dementia services. The Framework includes: a Joint Strategic Needs Assessment template; a summary of NICE and SCIE evidence for dementia services; commissioning levers against each of the NDS Objectives. To access the Framework click here
A Dementia Gateway was launched on 6 November 2009 by the Social Care Institute for Excellence to provide practical tips, tools and activities to help people in their work with dementia. You can visit the gateway at www.scie.org.uk/dementia.
An independent report commissioned by the DH concludes that inappropriate prescribing of antipsychotic drugs for people with dementia is widespread. The author, Dr Sube Banerjee, states 'It is clear from this review that the current level of use of antipsychotics for people with dementia presents a significant issue in terms of quality of care, with negative impacts in patient safety, clinical effectiveness and the patient experience.' Read the report here. |
Empowering Engagement: a stronger voice for older people
The Government response to John Elbourne's review
3 February 2009 |
The government has broadly supported the recommendations made by John Elbourne in his report examining older people's engagement with government at all levels, published 18 November 2008. It proposes to set up national leadership for older people in a UK Advisory Forum on Ageing to provide advice and support on the implementation and development of the Government's strategy for older people and an ageing society. It will also create a new structure with a designated lead regional coordinator for older people's engagement in each English region to help set up Regional Forums on Ageing where they do not already exist and it will continue to support OPAGs and other forums through Government Offices. To read the government response and proposals click here. |
The State of Social Care in England 2007-08
CSCI report
27 January 2009 |
The Commission for Social Care Inspection (CSCI) issued on 27 January 2009 its fourth and final report on the state of social care in England. The CSCI found that a year on from the publication of 'Putting People First' most people still experience a 'one-size-fits-all' model of care that is not geared towards people's individual needs. While there have been some tentative steps to address the new personalisation agenda, developments in social care are patchy and vary between different groups of people. Concerns remain about people who are 'lost to the system' because they are ineligible for publicly funded support or are 'self funders'. There continues to be tension between resourcing support for those with the highest levels of need and investing in a range of services which can maintain people's independence and improve their quality of life. To read the full report click here. |
Common Assessment Framework (CAF) for Adults
Demonstrator sites and results of consultation (updated 19 June 2009) |
The Department of Health held a consultation (22 January-17 April 2009)on improving the quality and efficiency of care and support for adults through improvements in the sharing and use of information. Topics covered the rationale for improving information, how assessment and care planning should be undertaken (the principles), what information should be commonly shared and with whom and the IT approaches that would enable this to take place within appropriate arrangements for consent, confidentiality and security. To access information on CAF for adults including information on demonstrator sites and results of the consultation click here. |
Strategy for Older People in Wales 2008-2013
Welsh Assembly Government |
Building on the achievements of the Strategy for Older People in Wales 2003-2008, phase 2 focuses on economic status, general well-being and independence of older people, around four themes:
- Valuing Older People - Maintaining and Developing Engagement. Promote positive images of ageing and ensure that the over 50s are able to participate as fully as they wish in their communities, giving them a stronger sense of engagement and influence.
-
Changing Society - The Economic Status and Contribution of Older People. Develop policies to increase the capacity of the over 50s to continue to work, learn, volunteer and care, making an active contribution for as long as they wish, and ensure that older people do not live in poverty.
-
Well Being and Independence. Improve the health and well being of older people through initiatives to promote health, as well as high quality, responsive and appropriately regulated health, social care and housing services.
-
Making it Happen - The Implementation of the Strategy. Implement the Strategy for Older People in Wales with support funding to ensure that it is a catalyst for change and innovation across all sectors, improving services for older people, providing the basis for effective planning for an ageing population and reflecting the concerns of older people.
Access the Strategies via the Welsh Assembly Government website here.
|
Preparing for Our Ageing Society: a discussion paper
25 November 2008 |
This discussion paper, and a series of associated public discussion events, are part of the first stage of a review of the government’s strategy for meeting the challenges of our ageing society. A consultation process to discuss the issues to be addressed in the strategy ran from 25 November 2008 to 20 January 2009 and responses to the discussion paper were published on 9 June 2009. To read the discussion paper and responses click here. |
Cutting the Cake Fairly
CSCI review of eligibility criteria for social care
22 October 2008 |
The Commission for Social Care Inspection (CSCI) issued on 22 October 2008 a report on eligibility criteria for social care. Tensions have developed between new approaches to personalisation and prevention and implementing the Fair Access to Care Services (FACS) framework, alongside councils' increasing tightening of their eligibility criteria. CSCI makes a series of recommendations to improve access to support consistent with 'Putting People First' and to provide some level of assistance and advice to everyone seeking care and support underpinned by the notion of progressive universalism. Click here to read the full report. |